Heart Block Poem
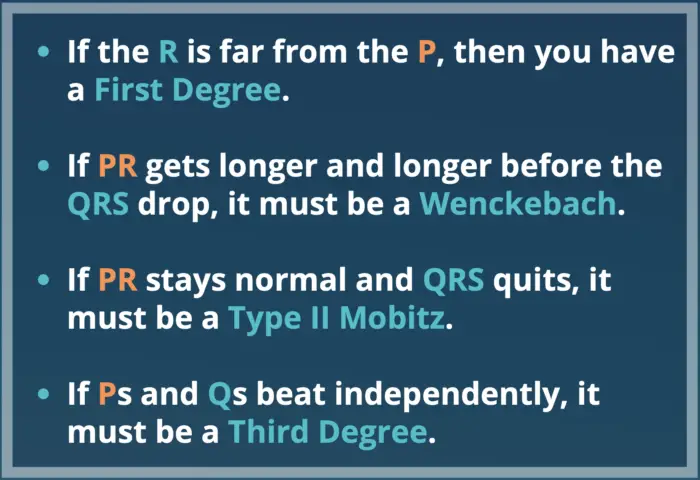
The heart block poem is:
If the R is far from the P, then you have a First Degree.
If PR gets longer and longer before the QRS drop, it must be a Wenckebach.
If PR stays normal and QRS quits, it must be a Type II Mobitz.
If Ps and Qs beat independently, it must be a Third Degree.
Atrioventricular (AV) heart blocks are conduction defects that impair the conduction of atrial impulses to ventricular pathways. There are three main types of AV heart blocks: first-degree, second-degree, and third-degree and the heart block poem can help you remember each one.
Second-degree heart blocks can be divided into 2 different types: Mobitz I (Wenckebach) and Mobitz II.
Heart Block Poem Cheat Sheet
Download this heart block poem cheat sheet or copy the images below to your phone.
1st Degree AV Heart Block
Catchphrase: First-Degree = Far away P
Poem: If the R is far from the P, then you have a first degree.
A first degree atrioventricular block displays the following characteristics:
- Heart rate between 60 and 100 BPM
- Prolonged PR interval greater than 0.20 seconds (200 msec)
- Normal QRS complex
- Regular heart rhythm
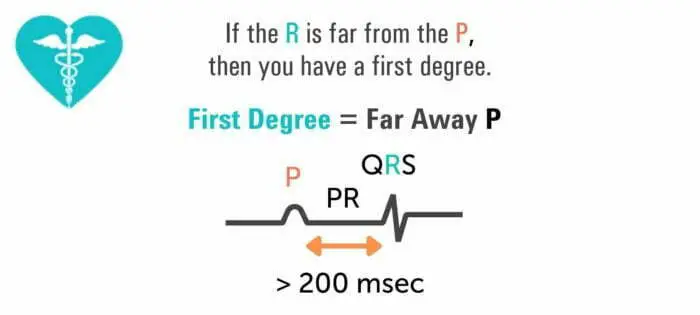
Typically, the delay occurs in the AV node. And despite the prolonged PR interval, every P wave is still followed by a QRS complex. No dropped or skipped beats occur with a first degree heart block.
In this case, every electrical signal is being transmitted from the atria to the ventricles but, the conduction through the AV node is slowed which creates the prolonged PR interval.
The first degree heart block is different than the second degree heart block and third degree heart block where a QRS complex isn't always present after each P wave.
The causes of a first degree block include:
- Hyperkalemia
- Hypokalemia
- Inferior wall MI or ischemia
- Calcium channel blockers or digoxin toxicity
- Use of antidysrhythmics and amiodarone
A first-degree AV heart block is an asymptomatic arrhythmia and must be treated by finding and treating the underlying cause. If healthcare workers detect the development of symptomatic bradycardia, or the PR interval is longer than 0.26 seconds, they should administer atropine.
To understand PR intervals, you must learn to read an ECG. Learning to read an ECG takes a lot of practice, and you will only fully get it when you look through hundreds of 12-lead ECG tracings.
2nd Degree AV Heart Block
There are 2 different types of second degree heart blocks: Mobitz I (Wenckebach) and Mobitz II.
Mobitz I or Type I Wenckebach
Catchphrase: Wenckebach = Longer Before Drop
Poem: If PR gets longer and longer before the QRS drop, it must be a Wenckebach.
To detect a second degree heart block, look for the following details in an ECG report:
- Regular atrial rhythm
- Irregular ventricular rhythm
- Atrial rate faster than the ventricular rate
- Progressively and slightly longer PR intervals until the QRS complex disappears
- Shorter PR interval after dropped heartbeat
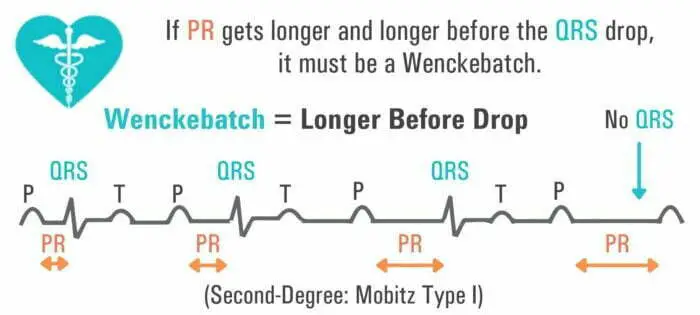
This part of the heart block poem refers to a PR interval that progressively lengthens with each beat until there is a QRS drop.
When a second degree heart block occurs, the conduction from the atria to the ventricles is progressively slowed with each beat, giving a prolonged PR interval. This persists until the atrial impulse is not conducted to the ventricles which results in a dropped QRS complex.
Conduction is then resumed after the dropped beat, and the sequence of events is repeated.
A second degree heart block is asymptomatic; however, it does have clinical manifestations. The patient may complain of weakness and vertigo and have an irregular pulse.
The condition is caused due to inferior wall MI and acute rheumatic fever. However, a second degree heart block can also appear after heart surgery and vagal stimulation. It is usually treated by treating the root cause, but atropine may be administered for management.
If symptomatic bradycardia appears, cardiologists can recommend implanting a temporary pacemaker. If appropriate, digoxin must be discontinued.
Mobitz II
A second-degree AV block Mobitz II has the same clinical manifestations as second-degree AV block Mobitz I. However, its characteristics on an ECG report are different:
- Regular atrial rhythm
- The ventricular rhythm may be regular or irregular, depending on the degree of the block
- Constant P-P interval
- QRS complex disappears or is periodically absent
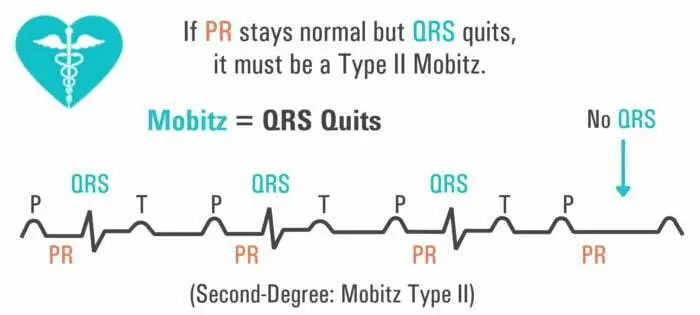
The segment of the heart block poem refers to a PR interval that remains constant with each beat, and then the QRS complex intermittently drops.
This occurs when each electrical signal is conducted at a constant rate from the atria to the ventricles, which shows a constant PR interval, but the atrial impulse is blocked intermittently and does not conduct to the ventricles resulting in a dropped QRS complex.
Mobitz type II blocks usually occur below the AV node (infranodal block).
The condition is caused by acute myocarditis, digoxin toxicity, anterior wall MI, or severe coronary artery disease.
Appropriate drugs such as epinephrine or dopamine may be administered if symptomatic bradycardia develops. A pacemaker may be installed if required. Digoxin must be discontinued if appropriate.
3rd Degree AV Heart Block
Also called a complete heart block, the characteristics of a third degree heart block on an ECG include:
- Regular atrial rhythm
- Regular ventricular rhythm (but slower than atrial rate)
- PR interval irregular
- P waves and QRS complexes have no relation
- QRS interval may be regular or abnormally wide and peculiar
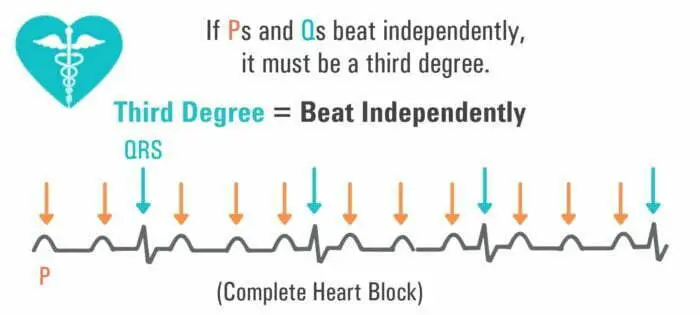
This last part of the heart block poem refers to a rhythm in which there is no relationship between the P waves and QRS complexes. This is what demonstrates that the patient has a third degree heart block which is considered a complete heart block.
When a third degree heart block occurs, the electrical signals between the atria and ventricles are completely blocked, resulting in no electrical communication between the two.
Cardiac function is maintained through a junctional escape rhythm in the ventricles. This rhythm allows the ventricles to depolarize and contract without receiving an electrical signal from the atria.
The arrhythmia clinically manifests as heart failure, hypotension, and angina. The possible causes include congenital abnormalities, digoxin toxicity, hypoxia, MI, rheumatic fever, and Lev's disease.
A pacemaker can help manage the condition, but nurses may administer dopamine or epinephrine if bradycardia occurs.
Differential Diagnosis for Shortened and Prolonged PR Interval
The first step to determining the differential for an abnormal PR interval begins by excluding the abnormality considering normal PR variability. After this is done, a diagnostic algorithm is used based on the length of the PR interval.
Normal PR Variability
The PR interval can vary with the heart rate in a normal physiologic state. This is caused by the variations in sympathetic tone.
An increased tone makes for increased conduction at a faster heart rate. In contrast, the withdrawal of the sympathetic tone slows conduction.
But regardless of these variations in physiology, a normal PR interval lies between 140 ms and 200 ms. Young adults and athletes sometimes have a PR interval longer than 200 ms for physiologic reasons.
Administering atropine shortens the PR interval; however, this doesn't work for patients with an underlying pathophysiologic cardiac disease.
PR Interval < 0.12 s
If the PR interval is shorter than 120 ms, the diagnosis is limited mainly to the existence of a bypass tract between the ventricles and the atria. The PR interval tends to be shorter since the cardiac current bypasses the AV node and travels directly between the ventricles and atria (WPW).
However, the bypass tract may also exist between the AV node and the atria.
PR Interval > 0.2 s
Typically, patients that have isolated instances of prolonged PR intervals are asymptomatic. That said, prolonged PR intervals are sometimes associated with a high-grade AV block. In this case, the patient may experience symptoms such as fatigue, frank syncope, and decreased exercise tolerance.
Patients whose ECGs have a prolonged PR interval tend to be older with a history of cardiovascular disease. That said, young adults and athletes sometimes have asymptomatic PR prolongation.
To sum up, a prolonged PR interval can be caused by a first-degree heart block or second-degree heart block of Mobitz Type I or Mobitz Type II.
Management of Abnormal PR Interval
Management of a shortened or prolonged PR interval varies by state and whether it is acute or chronic.
Management of Shortened PR Interval
Acute
A patient with a bypass tract may have supraventricular tachycardia. In patients that suffer from atrioventricular reentrant tachycardia during atrial fibrillation, the ventricles can get excited ahead of time. This increases the risk of ventricular fibrillation.
For this reason, patients with history or evidence of pre-excitation should not be administered nodal agents. Attempting to control their heart rate by this means can make their arrhythmia worse and is often fatal.
Chronic
Those with a short PR interval can be diagnosed solely with the ECG report. That said, the emphasis must be placed on assessing whether the patient has any associated symptomatic tachycardia that indicates the existence of an accessory pathway.
If a patient has symptomatic tachycardias, they must see a cardiologist quickly so they can evaluate their condition correctly and suggest treatment options. Depending on the circumstance, the cardiologist may recommend getting radiofrequency ablation.
The risk of sudden cardiac death in patients with an accessory pathway having an asymptomatic tachycardia is low. However, the risks aren't the same for every patient. Only a cardiologist can evaluate the risk and suggest the right option.
Management of Prolonged PR Interval
The management practices of a prolonged PR depend on the degree of heart blockage. In a first-degree heart block, typically, no interventions are made.
Second-degree heart block typically develops due to reversible causes. In emergencies, the management approach aims to increase the heart rate without affecting the underlying cause. In the case of a Mobitz I block, if the heart rate is higher than 40 and the patient doesn't have any symptoms, intervention is not necessary.
On the other hand, if the HR is lower than 40 and the patient has symptoms, 0.5 mg Atropine is typically administered. Up to three doses are given in the interval of three to five minutes, so the heart conducts more impulses through the AV node.
If the symptomatic patient is experiencing a heart block due to a reversible cause, a temporary pacemaker may be implanted until the reversible cause is addressed. A permanent pacemaker may be implanted in patients with irreversible causes.
A Mobitz II block is more likely to appear due to an irreversible cause. While the emergency management options for this kind of block are the same as the options for a Mobitz I block, Mobitz II blocks have a higher chance of developing into complete heart blocks. For this reason, patients typically require the insertion of a permanent pacemaker.
Summary
Check out the discussion about the heart block poem over on reddit.
