EKG Interpretation Cheat Sheet
Electrocardiograms (known as EKG or ECG) stand among the most commonly used diagnostic tools in medicine. In this post, I cover how the tool works and provide a printable EKG interpretation cheat sheet you can keep with you during training to help learn to identify various conditions.
For other nursing tips, check out the BUBBLE HE mnemonic along with VEAL CHOP, HELLP, and LARA CROFT.
How Does an EKG Work?
An electrocardiogram is a painless, non-invasive way to help diagnose many common heart problems in people of all ages. To perform an EKG, the machine’s electrodes are attached to the patient’s skin. The electrodes then measure the current moving through the heart, which the machine interprets as waveforms. The waveforms are displayed on the machine’s display.
The electrical impulses in the heart are responsible for stimulating and coordinating atrial and ventricular myocardial contractions. These contractions are responsible for pumping the blood in and out of the heart.
What is a Dysrhythmia or Arrhythmia?
Dysrhythmia or arrhythmia are disturbances in the heart’s normal rhythm, occurring due to changes in the conduction of electric impulses within the heart.
Here’s an EKG interpretation cheat sheet that sums up all of the arrhythmias in a manner that’s easy to understand.
EKG Interpretation Cheat Sheet
EKG interpretation can seem complicated, but experienced doctors and various types of nurses can do it with ease. These healthcare professionals can differentiate between conditions like atrial fibrillation and tachycardia because they’ve practiced EKG interpretation rigorously.
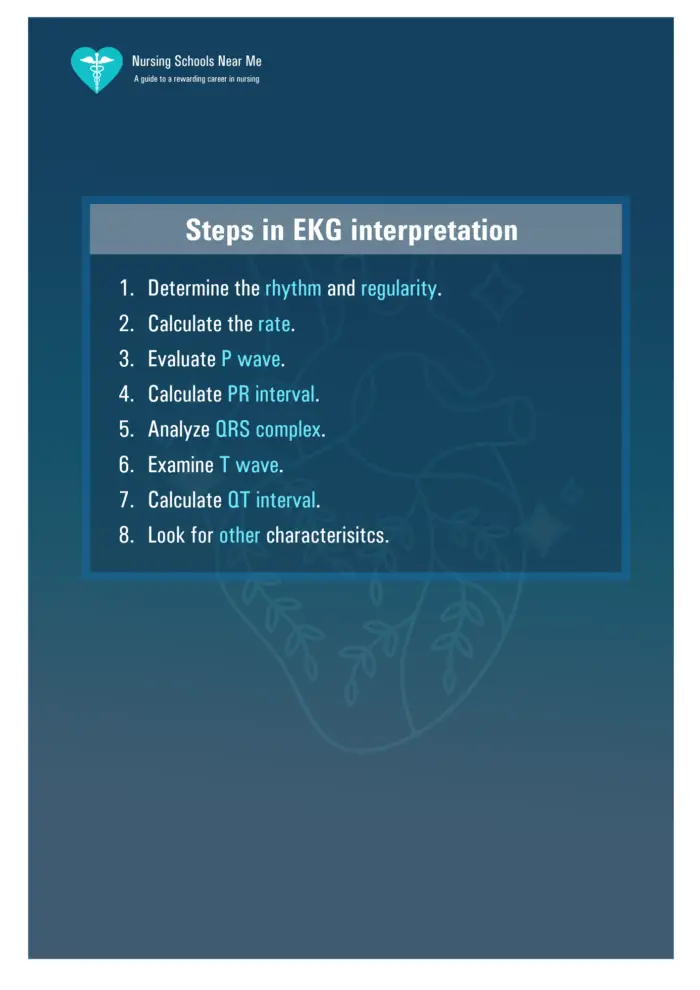
Besides having a solid theoretical foundation and a keen eye, interpreting EKG readings to detect heart arrhythmias takes many hours of practice. There are several steps involved in EKG interpretation.
Interpreting the EKG involves checking the heart frequency and rhythm, electrical heart axis, PR interval, and QRS complex. For EKG interpretation, you must also check the repolarization and R/S ratio to determine whether there’s a heart arrhythmia and of what kind.
Regardless of the role you play in the healthcare system, after practicing interpreting EKG a few times with the help of this EKG interpretation cheat sheet, interpreting EKG should become second nature.
Download or print the PDF cheat sheet for EKG interpretation below. Or, click on the images and save them directly to your mobile device.
Simply click on each image and save.
Sinus Tachycardia
Sinus tachycardia is a condition that originates from the sinus node, and the heart rate is consistently over 100 beats per minute.
- Heart rate ranging between 100 and 180 BPM
- There are P waves before every QRS complex
- Normal PR intervals
- Normal QRS complexes
- Heart rhythm is normal
- Conduction is regular
There are several possible causes of sinus tachycardia. Anxiety, fever, drugs, exercise, anemia, hypovolemia, shock, and heart failure may cause these arrhythmias.
Typically, the condition is asymptomatic and is revealed during checkups. While the heart rate is reduced using a beta-blocker or carotid massage, treatment is typically directed at the condition’s root cause.
Sinus Bradycardia
Like Sinus Tachycardia, Sinus Bradycardia originates from the sinoatrial node. The difference between the two conditions is that in Sinus Bradycardia, the heart rate is less than 60 BPM.
When you get around to EKG interpretation, these are the characteristics you will observe for this condition:
- Heart rate <60 BPM
- There are P waves before every QRS complex
- Heart rhythm is regular
- Conduction is normal
- Normal PR interval
- Normal QRS complex
Possible causes of sinus bradycardia include drug use, hypothermia, vagal stimulation, and sinus node involvement in myocardial infarction. Athletes tend to have this arrhythmia since they have quality stroke volume.
Like Sinus Tachycardia, Sinus Bradycardia is typically asymptomatic. However, it may manifest as fatigue, dizziness, and syncope.
Besides treatment of the root cause, the arrhythmia is managed by administering anticholinergic drugs such as atropine sulfate.
Premature Atrial Contraction
These are ectopic heartbeats that originate from the atria. These are not rhythms and occur when the cells in the heart fire before the heart is normally supposed to beat. Premature atrial contractions are commonly called heart palpitations.
The condition has the following characteristics:
- Premature P waves that look abnormal
- Very early or blocked PACs will show no QRS complex after P waves
- Most P waves buried in the preceding T wave
Atrial ischemia, coronary or valvular heart disease, heart failure, COPD, hypoxia, and electrolyte imbalance can cause PAC. Treatment is typically not required; however, healthcare professionals may administer antidysrhythmic drugs or carotid sinus massage.
Atrial Flutter
These are abnormal rhythms occurring at the atria of the heart. While the atrial rhythm is regular in this condition, the atrial rate is between 250 and 400 beats per minute. This gives the EKG a sawtooth appearance.
Further, the QRS complexes are irregular in rate but uniform in shape.
The causes of atrial flutter include heart failure, mitral valve or tricuspid valve disease, cor pulmonale, pulmonary embolism, carditis, inferior wall MI, and dioxin toxicity.
If the patient has a ventricular rate greater than 150BPM, you must prepare for immediate cardioversion. But this is not necessary if the patient is stable. Drug therapy using calcium channel blockers, beta-adrenergic blockers, or antiarrhythmic drugs may be administered.
Atrial flutter causes pooling of blood in atria, so anticoagulation may be necessary.
Atrial Fibrillation
Uncoordinated and disorganized twitching of the atrial musculature is called atrial fibrillation. The rapid production of atrial impulses causes it.
The EKG interpretation of atrial fibrillation has the following characteristics:
- Atrial rate: 350 – 600 BPM
- Ventricular rate: 120 – 200 BPM
- P wave with indiscernible due to irregular baseline
- PR interval immeasurable
- Normal QRS complex
- Rapid and irregular heart rhythm unless controlled
Atrial fibrillation may be caused by:
- Congenital heart disease
- Atherosclerosis
- Chronic obstructive pulmonary disease
- Heart failure
- Hypothyroidism
- Thyrotoxicosis
While atrial fibrillation is typically asymptomatic, its clinical manifestations may appear as palpitations, pulmonary edema, or dyspnea.
Nurses must administer the prescribed treatment to reduce atrial irritability, decrease the ventricular response, and eliminate the arrhythmia’s underlying cause.
Premature Junctional Contraction
In PJC, some parts of the heart become more excitable than usual.
The EKG interpretation of the Premature Junctional Contraction has the following characteristics:
- Inverted P wave
- Irregular atrial and ventricular rhythms
- If P wave precedes QRS complex, the PR interval is shorter than 0.12 seconds
- Normal QRS complex
PJC may be caused by myocardial ischemia or infarction, excessive caffeine use, excessive amphetamine use, and digoxin toxicity.
Treatment includes correction of the underlying cause and discontinuation of the digoxin if appropriate.
Atrioventricular Blocks
These are conduction defects in the AV junction that impair the conduction of atrial impulses to the ventricular pathways. AV blocks are of three types.
Copy our cheat sheet and learn the heart block poem to make it easy to identify the AV blocks below.
First Degree AV Block
- Heart rate between 60 and 100 BPM
- Prolonged PR intervals, typically 0.20 seconds long
- Normal QRS complex
- Regular heart rhythm
A first-degree AV block may be caused by:
- Hyperkalemia
- Hypokalemia
- Inferior wall MI or ischemia
- Calcium channel blockers or digoxin toxicity
- Use of antidysrhythmics and amiodarone
The arrhythmia is asymptomatic. The underlying cause must be treated to treat the arrhythmia. If symptomatic Bradycardia develops or PR interval exceeds 0.26 seconds, administer atropine.
Second Degree AV Block Mobitz I
To detect second degree AV block mobitz I, look for the following characteristics during EKG interpretation:
- Regular atrial rhythm
- Irregular ventricular rhythm
- Atrial rate faster than the ventricular rate
- Progressively and slightly longer PR intervals until the QRS complex disappears
- Shorter PR interval after dropped heartbeat
While the condition is asymptomatic, its clinical manifestations include weakness, vertigo, and an irregular pulse. It may be caused by cardiac surgery, inferior wall MI, or acute rheumatic fever. Vagal stimulation is also a possible cause.
Correction of the cause is the primary treatment option; however, atropine may be administered. If symptomatic Bradycardia appears, a pacemaker may be installed temporarily. Digoxin must be discontinued if appropriate.
Second Degree AV Block Mobitz II
The clinical manifestations of this condition are the same as Mobitz I, but its EKG characteristics are different:
- Regular atrial rhythm
- The ventricular rhythm may be regular or irregular, depending on the degree of the block
- Constant P-P interval
- QRS complex disappears or is periodically absent
Mobitz II may be caused by severe coronary artery disease, anterior wall MI, acute myocarditis, or digoxin toxicity. If symptomatic Bradycardia develops, atropine, epinephrine, or dopamine may be administered. Installation of a pacemaker is also an option. Digoxin may be discontinued if appropriate.
Third Degree AV Block
The third-degree AV block is a complete heart block. The EKG interpretation characteristics include:
- Regular atrial rhythm
- Regular ventricular rhythm (but slower than atrial rate)
- PR interval irregular
- P waves and QRS complexes have no relation
- QRS interval may be regular or abnormally wide and peculiar
Third-degree AV blocks may be caused by rheumatic fever, hypoxia, MI, congenital abnormalities, digoxin toxicity, and Lev’s disease.
Clinical manifestations of this arrhythmia include heart failure, hypotension, and angina. Installation of a pacemaker may be considered to manage the condition, but for Bradycardia, epinephrine, dopamine, or atropine is administered.
Premature Ventricular Contractions
Increased automaticity of ventricular muscle cells causes early ventricular contractions.
While these aren’t considered harmful, they can be concerning if they occur:
- More than six times within one minute
- In sets of two or three
- Near a T wave
- As multifocal
The characteristics of PVCs in EKG interpretation are:
- Regular atrial rhythm
- Regular ventricular rhythm
- Wide and distorted QRS complex, typically longer than 0.14 seconds
- Premature QRS complex, thenceforward a complete pause
- Early QRS complex occurring individually, in sets of two, or triplets
Palpitations, lightheadedness, and palpitations are all clinical manifestations of PVCs, but they are often asymptomatic.
Premature ventricular tachycardia may cause ventricular tachycardia or fibrillation. For treatment, antiarrhythmic medication is administered.
Ventricular Tachycardia
Three or more consecutive premature ventricular contractions are termed Ventricular Tachycardia. The condition is considered a medical emergency since the decreased diastolic filling leads to the unsustainability of cardiac output.
To detect VT, look for these characteristics during EKG interpretation:
- Heart rate between 100 and 250 BPM
- Blurred P wave in the QRS complex; but the P wave is unrelated to QRS complex
- No PR interval present
- T wave in the opposite direction; wide and abnormal QRS complex
- Regular heart rhythm
- The heart may stop and start suddenly
Dyspnea, lightheadedness, unconsciousness, and weakness are clinical manifestations of ventricular tachycardia.
VT can be caused by:
- Myocardial infarction
- CAD
- Mitral valve prolapse
- Aneurysm
- Rheumatic heart diseases
- Pulmonary embolism
- Hyperkalemia and hypokalemia
Anxiety is also known to cause the condition.
Managing Ventricular Tachycardia with Pulse
If the patient is hemodynamically stable, ACLS protocol must be followed and amiodarone administered. If amiodarone is ineffective, synchronized cardioversion must be initiated.
Managing Pulseless Ventricular Tachycardia
Initiate CPR, and follow ACLS protocol for defibrillation. ET intubation is done next, along with the administration of epinephrine or vasopressin.
Ventricular Fibrillation
It is the rapid and ineffective quivering of ventricles.
It can be rapidly fatal. Its EKG characteristics include:
- Rapid and uncoordinated heart rate, with ineffective contractions
- Chaotic heart rhythm
- No P wave
- No PR interval
- Wide and irregular QRS complexes
Ventricular fibrillation is typically caused by myocardial ischemia or infarction. However, it can also result from electrolyte imbalances, ventricular tachycardia, hypothermia, and quinidine or digoxin toxicity.
The condition clinically manifests as loss of consciousness or blood pressure, pulselessness, seizures, cessation of respiration, and sudden death.
ACLS protocol must be followed for defibrillation, ET intubation, and vasopressin or epinephrine administration to manage ventricular fibrillation.
Other Arrhythmias
Atrial Tachycardia
In addition to aiding with the diagnosis of atrial tachycardia, EKG machines can also help determine the origin of focal tachycardia.
The characteristics of this arrhythmia include:
- Atrial rate ranging between 100 BPM and 250 BPM
- Variable ventricular conduction, which is:
- Regular if there is a 1 to 1, 2 to 1, or 4 to 1 AV block
- Irregular or irregularly irregular if there is a variable AV block
- The P wave is unifocal but similar in morphology
- The P wave is abnormal and may be inverted
- Possibility of either long RP or short PR intervals
- The heart rhythm may be sustained or paroxysmal:
- May increase in the rate of initiation
- May decrease in the rate of termination
More commonly, this arrhythmia occurs in individuals with heart disease that may or may not have suffered heart failure. It also occurs in individuals with ischemic coronary artery disease.
But the focal atrial tachycardia can also occur in healthy individuals that do not have heart disease. Possible causes include hypoxia, heightened sympathetic tone, stimulant use (caffeine, chocolate, cocaine, ephedra), metabolic disturbance, alcohol use, and digoxin toxicity.
Initial arrhythmia management must address the root causes. The ventricular rate can be controlled using beta or calcium channel blockers.
However, if the arrhythmia persists and the patient is symptomatic, IA, IC, or III antiarrhythmic medication may be administered.
For patients failing medical therapy, catheter ablation can be considered.
Torsade de Pointes
During EKG interpretation of this arrhythmia, you will detect:
- Heart rate between 200 and 250 beats per minute
- Undulating QRS axis
- Long QT interval (averages about 0.44 seconds) but may vary by sex
The torsades de pointes VT typically results from class Ia, Ic, or III antiarrhythmic drug administration. However, phenothiazines, tricyclic antidepressants, and specific antiviral and antifungal medication may induce this VT. A family history of VT suggests a congenital syndrome.
Treatment of the cause, correction of electrolyte abnormalities, magnesium sulfate IV administration, and unsynchronized DC cardioversion can help manage the condition.
Supraventricular Tachycardia
SVT is an atrial tachycardia that is not under direct control from the SA node. Instead, the impulses come from tissues around the atrioventricular node.
This arrhythmia can occur in all age groups, and the EKG characteristics are:
- Regular rhythm
- Heart rate between 140 and 220 BPM
- Normal QRS complexes
- P wave typically buried in the preceding T wave
- PR interval depends on the position of the SVT pacemaker
Clinical manifestations of SVT include heart palpitations, rapid heartbeat, weakness, chest pain, breathlessness, dizziness, fainting, sweating, and a pounding sensation in the neck.
While this arrhythmia does not require treatment, adenosine is administered as first-line treatment.
EKG Interpretation Cheat Sheet: Summed Up
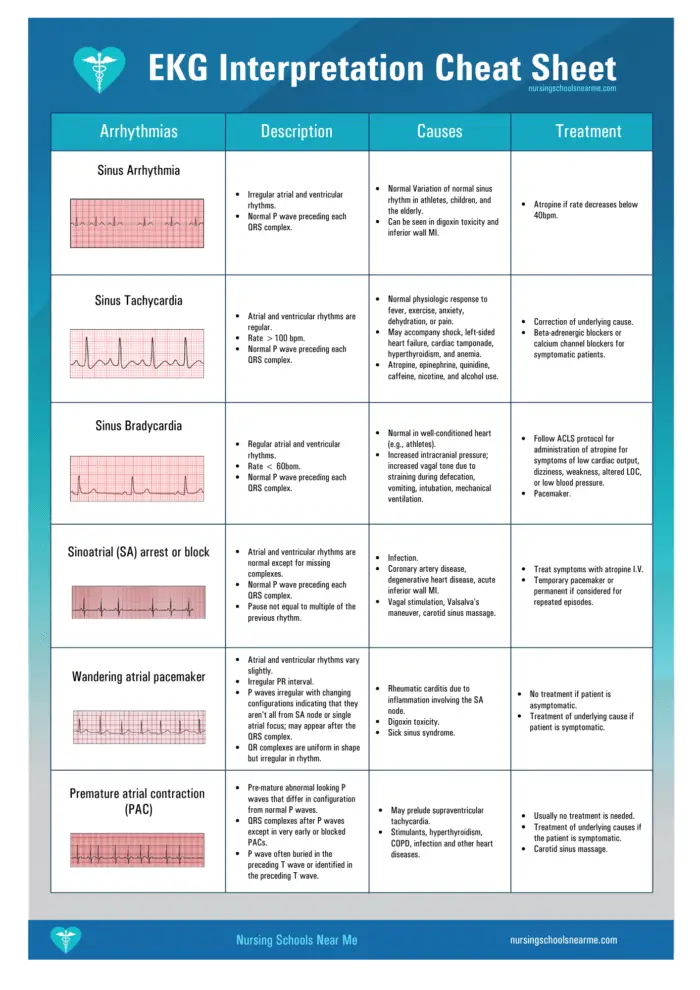
| Arrhythmias | Description | Causes | Treatment |
|---|---|---|---|
| Sinus Arrhythmia | Irregular atrial and ventricular rhythms. Normal P wave preceding each QRS complex. | Normal variation of normal sinus rhythm in athletes, children, and the elderly. Can be seen in digoxin toxicity and inferior wall MI. | Atropine if rate decreases below 40 bpm. |
| Sinus Tachycardia | Atrial and ventricular rhythms are regular. Rate > 100 bpm. Normal P wave preceding each QRS complex. | Normal physiologic response to fever, exercise, anxiety, dehydration, or pain. May accompany shock, left-sided heart failure, cardiac tamponade, hyperthyroidism, and anemia. Atropine, epinephrine, quinidine, caffeine, nicotine, and alcohol use. | Correction of underlying cause. Beta-adrenergic blockers or calcium channel blockers for symptomatic patients. |
| Sinus Bradycardia | Regular atrial and ventricular rhythms. Rate < 60 bpm. Normal P wave preceding each QRS complex. | Normal in a well-conditioned heart (e.g., athletes). Increased intracranial pressure; increased vagal tone due to straining during defecation, vomiting, intubation, mechanical ventilation. | Follow ACLS protocol for administration of atropine for symptoms of low cardiac output, dizziness, weakness, altered LOC, or low blood pressure. Pacemaker. |
| Sinoatrial (SA) arrest or block | Atrial and ventricular rhythms normal except for missing complex. Normal P wave preceding each QRS complex. Pause not equal to multiple of the previous rhythm. | Infection. Coronary artery disease, degenerative heart disease, acute inferior wall MI. Vagal stimulation, Valsalva’s maneuver, carotid sinus massage. | Treat symptoms with atropine I.V. Temporary pacemaker or permanent pacemaker if considered for repeated episodes. |
| Wandering atrial pacemaker | Atrial and ventricular rhythms vary slightly. Irregular PR interval. P waves irregular with changing configurations indicating that they aren’t all from SA node or single atrial focus; may appear after the QRS complex. QRS complexes uniform in shape but irregular in rhythm. | Rheumatic carditis due to inflammation involving the SA node. Digoxin toxicitySick sinus syndrome | No treatment if patient is asymptomatic. Treatment of underlying cause if patient is symptomatic. |
| Premature atrial contraction (PAC) | Premature, abnormal-looking P waves that differ in configuration from normal P waves. QRS complexes after P waves except in very early or blocked PACs. P wave often buried in the preceding T wave or identified in the preceding T wave. | May prelude supraventricular tachycardia. Stimulants, hyperthyroidism, COPD, infection, and other heart diseases. | Usually no treatment is needed. Treatment of underlying cause if patient is symptomatic. Carotid sinus massage. |
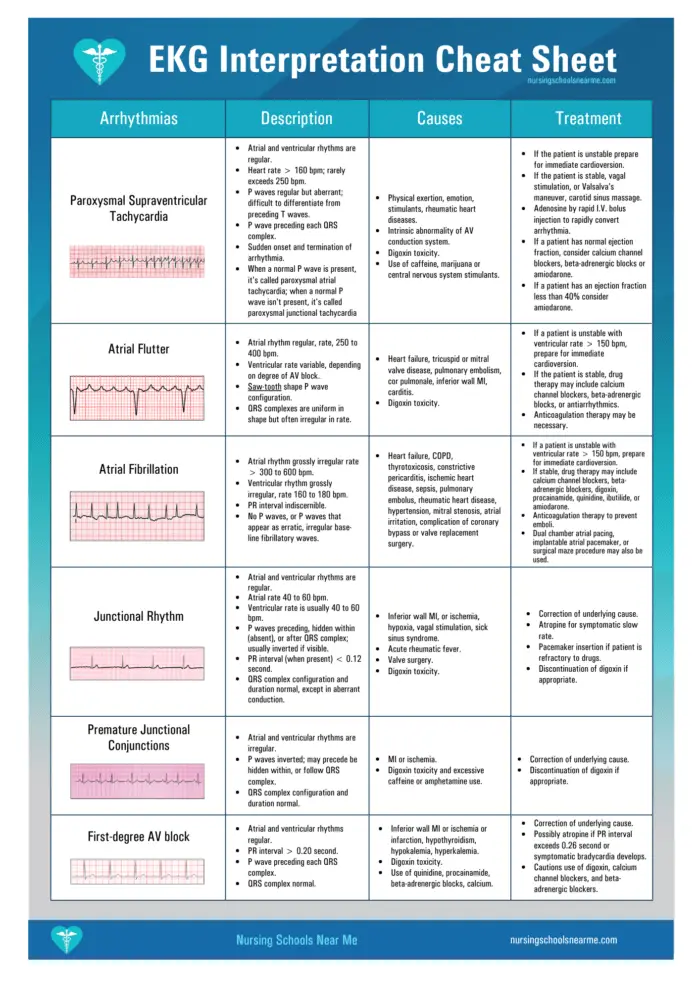
| Paroxysmal Supraventricular Tachycardia | Atrial and ventricular rhythms are regular. Heart rate > 160 bpm; rarely exceeds 250 bpm. P waves regular but aberrant; difficult to differentiate from preceding T wave. P wave preceding each QRS complex. Sudden onset and termination of arrhythmia. When a normal P wave is present, it’s called paroxysmal atrial tachycardia; when a normal P wave isn’t present, it’s called paroxysmal junctional tachycardia. | Physical exertion, emotion, stimulants, rheumatic heart diseases. Intrinsic abnormality of AV conduction system. Digoxin toxicity. Use of caffeine, marijuana, or central nervous system stimulants. | If patient is unstable prepare for immediate cardioversion. If patient is stable, vagal stimulation, or Valsalva’s maneuver, carotid sinus massage. Adenosine by rapid I.V. bolus injection to rapidly convert arrhythmia. If patient has normal ejection fraction, consider calcium channel blockers, beta-adrenergic blocks, or amiodarone. If patient has an ejection fraction less than 40%, consider amiodarone. |
| Atrial flutter | Atrial rhythm regular, rate, 250 to 400 bpm. Ventricular rate variable, depending on degree of AV block. Saw-tooth shape P wave configuration. QRS complexes uniform in shape but often irregular in rate. | Heart failure, tricuspid or mitral valve disease, pulmonary embolism, cor pulmonale, inferior wall MI, carditis. Digoxin toxicity. | If patient is unstable with ventricular rate > 150bpm, prepare for immediate cardioversion. If patient is stable, drug therapy may include calcium channel blockers, beta-adrenergic blocks, or antiarrhythmic. Anticoagulation therapy may be necessary. |
| Atrial Fibrillation | Atrial rhythm grossly irregular rate > 300 to 600 bpm. Ventricular rhythm grossly irregular, rate 160 to 180 bpm. PR interval indiscernible. No P waves, or P waves that appear as erratic, irregular base-line fibrillatory waves | Heart failure, COPD, thyrotoxicosis, constrictive pericarditis, ischemic heart disease, sepsis, pulmonary embolus, rheumatic heart disease, hypertension, mitral stenosis, atrial irritation, complication of coronary bypass or valve replacement surgery. | If patient is unstable with ventricular rate > 150bpm, prepare for immediate cardioversion. If stable, drug therapy may include calcium channel blockers, beta-adrenergic blockers, digoxin, procainamide, quinidine, ibutilide, or amiodarone. Anticoagulation therapy to prevent emboli. Dual chamber atrial pacing, implantable atrial pacemaker, or surgical maze procedure may also be used. |
| Junctional Rhythm | Atrial and ventricular rhythms are regular. Atrial rate 40 to 60 bpm. Ventricular rate usually 40 to 60 bpm. P waves preceding, hidden within (absent), or after QRS complex; usually inverted if visible. PR interval (when present) < 0.12 secondQRS complex configuration and duration normal, except in aberrant conduction. | Inferior wall MI, or ischemia, hypoxia, vagal stimulation, sick sinus syndrome. Acute rheumatic fever. Valve surgeryDigoxin toxicity. | Correction of underlying cause. Atropine for symptomatic slow rate. Pacemaker insertion if patient is refractory to drugs. Discontinuation of digoxin if appropriate. |
| Premature Junctional Conjunctions | Atrial and ventricular rhythms are irregular. P waves inverted; may precede be hidden within, or follow QRS complex. QRS complex configuration and duration normal. | MI or ischemia. Digoxin toxicity and excessive caffeine or amphetamine use. | Correction of underlying cause. Discontinuation of digoxin if appropriate. |
| First-degree AV block | Atrial and ventricular rhythms regular. PR interval > 0.20 second. P wave preceding each QRS complex. QRS complex normal. | Inferior wall MI or ischemia or infarction, hypothyroidism, hypokalemia, hyperkalemia. Digoxin toxicity. Use of quinidine, procainamide, beta-adrenergic blockers, calcium | Correction of the underlying cause. Possibly atropine if PR interval exceeds 0.26 second or symptomatic bradycardia develops. Cautious use of digoxin, calcium channel blockers, and beta-adrenergic blockers. |
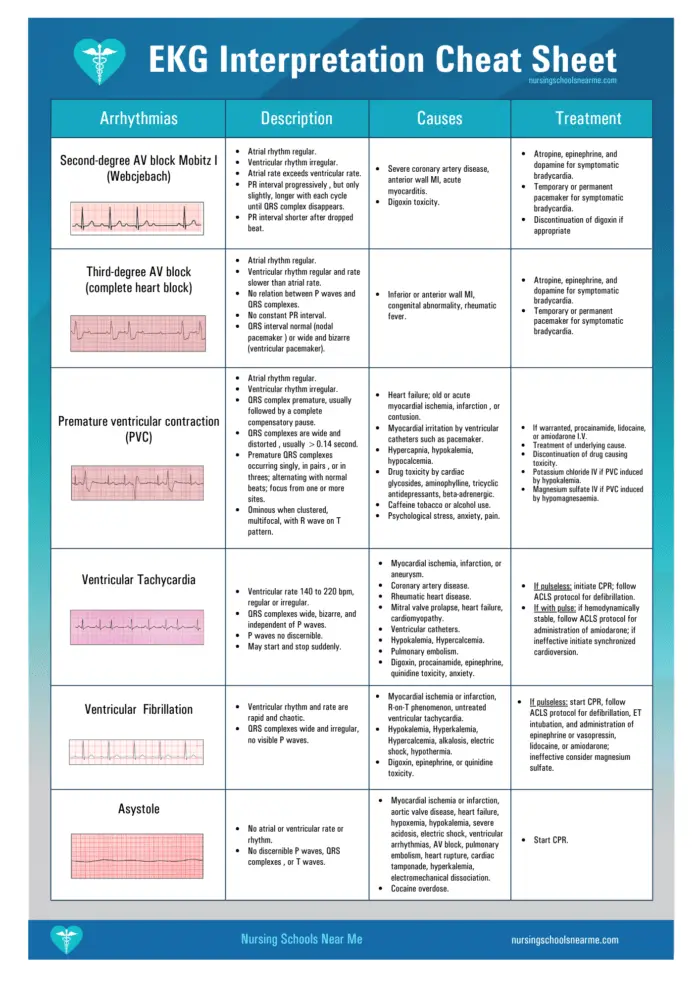
| Second-degree AV block Mobitz I (Wenckebach) | Atrial rhythm regular. Ventricular rhythm irregular. Atrial rate exceeds ventricular rate. PR interval progressively, but only slightly, longer with each cycle until QRS complex disappears. PR interval shorter after dropped beat. | Severe coronary artery disease, anterior wall MI, acute myocarditis. Digoxin toxicity. | Atropine, epinephrine, and dopamine for symptomatic bradycardia. Temporary or permanent pacemaker for symptomatic bradycardia. Discontinuation of digoxin if appropriate. |
| Third-degree AV block (complex heart block) | Atrial rhythm regular. Ventricular rhythm regular and rate slower than atrial rate. No relation between P waves and QRS complexes. No constant PR interval. QRS interval normal (nodal pacemaker) or wide and bizarre (ventricular pacemaker). | Inferior or anterior wall MI, congenital abnormality, rheumatic fever. | Atropine, epinephrine, and dopamine for symptomatic bradycardia. Temporary or permanent pacemaker for symptomatic bradycardia. |
| Premature ventricular contraction (PVC) | Atrial rhythm regular. Ventricular rhythm irregular. QRS complex premature, usually followed by a complete compensatory pause. QRS complex wide and distorted, usually >0.14 second. Premature QRS complexes occurring singly, in pairs, or in threes; alternating with normal beats; focus from one or more sites. Ominous when clustered, multifocal, with R wave on T pattern. | Heart failure; old or acute myocardial ischemia, infarction, or contusion. Myocardial irritation by ventricular catheters such as a pacemaker. Hypercapnia, hypokalemia, hypocalcemia. Drug toxicity by cardiac glycosides, aminophylline, tricyclic antidepressants, beta-adrenergic. Caffeine, tobacco, or alcohol use. Psychological stress, anxiety, pain | If warranted, procainamide, lidocaine, or amiodarone I.V. Treatment of underlying cause. Discontinuation of drug causing toxicity. Potassium chloride IV if PVC induced by hypokalemia. Magnesium sulfate IV if PVC induced by hypomagnesemia. |
| Ventricular Tachycardia | Ventricular rate 140 to 220 bpm, regular or irregular. QRS complexes wide, bizarre, and independent of P waves. P waves not discernible. May start and stop suddenly. | Myocardial ischemia, infarction, or aneurysm. Coronary artery disease. Rheumatic heart disease. Mitral valve prolapse, heart failure, cardiomyopathyVentricular catheters. Hypokalemia, Hypercalcemia. Pulmonary embolism. Digoxin, procainamide, epinephrine, quinidine toxicity, anxiety. | If pulseless: initiate CPR; follow ACLS protocol for defibrillation. If with pulse: If hemodynamically stable, follow ACLS protocol for administration of amiodarone; if ineffective initiate synchronized cardioversion. |
| Ventricular Fibrillation | Ventricular rhythm and rate are rapid and chaotic. QRS complexes wide and irregular, no visible P waves | Myocardial ischemia or infarction, R-on-T phenomenon, untreated ventricular tachycardia, hypokalemia, hyperkalemia, hypercalcemia, alkalosis, electric shock, hypothermia. Digoxin, epinephrine, or quinidine toxicity. | If pulseless: start CPR, follow ACLS protocol for defibrillation, ET intubation, and administration of epinephrine or vasopressin, lidocaine, or amiodarone. If ineffective consider magnesium sulfate. |
| Asystole | No atrial or ventricular rate or rhythm. No discernible P waves, QRS complexes, or T waves | Myocardial ischemia or infarction, aortic valve disease, heart failure, hypoxemia, hypokalemia, severe acidosis, electric shock, ventricular arrhythmias, AV block, pulmonary embolism, heart rupture, cardiac tamponade, hyperkalemia, electromechanical dissociation. Cocaine overdose. | Start CPR. |