Patient Positioning: Everything You Need to Know [Cheat Sheet]

Appropriate patient positioning helps ensure that a surgical procedure is effective. Patient positioning depends on factors such as the type and length of procedure, required equipment, and anesthesia access to the patient. Safe patient positioning is the responsibility of the entire medical team in the OT and particularly the OR nurse.
Correct patient positioning also ensures that the patients are safe during their recovery after surgery. In this post, we discuss all the different patient positions, guidelines for properly positioning patients, and also provide a patient positioning cheat sheet.
What is Patient Positioning?
Patient positioning involves maintaining neutral body alignment per the requirements of the procedure. It is accomplished by preventing hyperextension and excessive lateral rotation.
Positioning patients correctly is an essential aspect of nursing since it helps prevent injury and complications of immobility. Appropriate patient positioning optimally exposes the area treatment area and avoids unnecessary exposure.
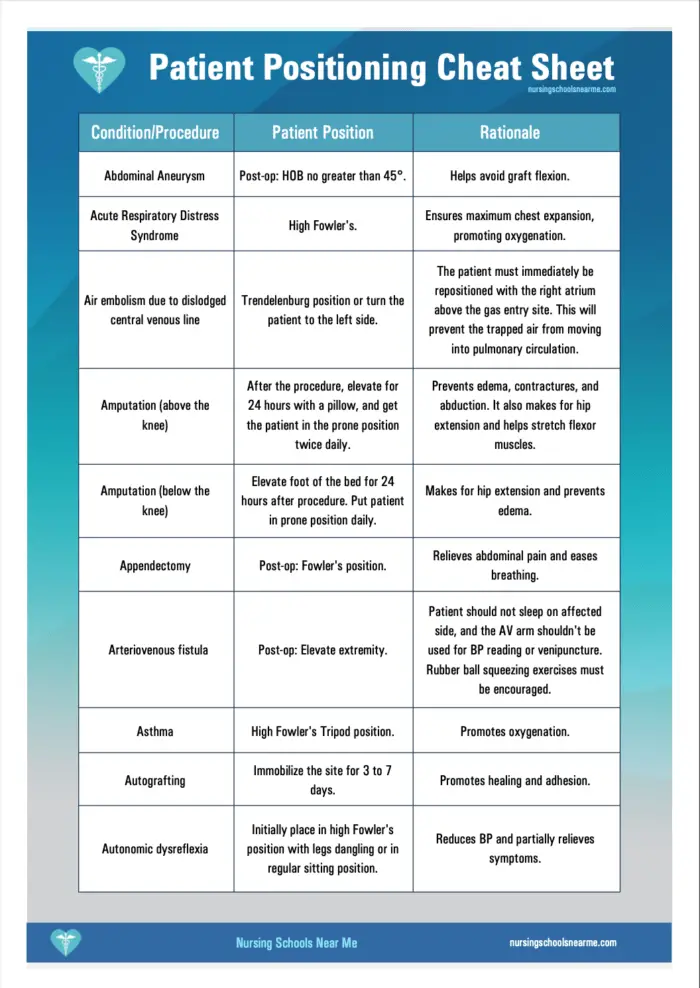
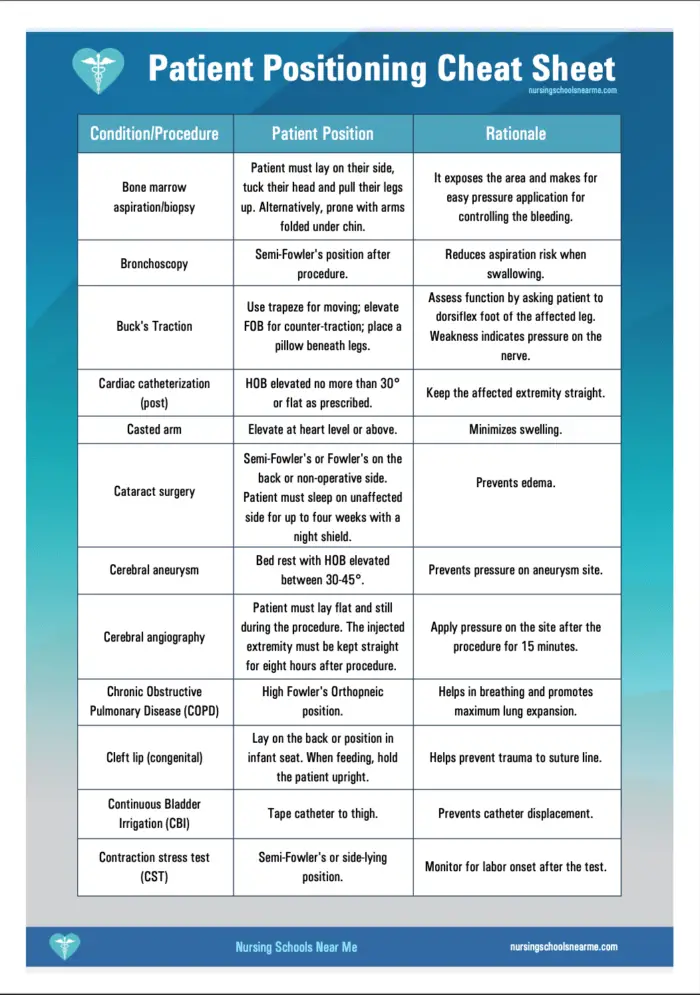
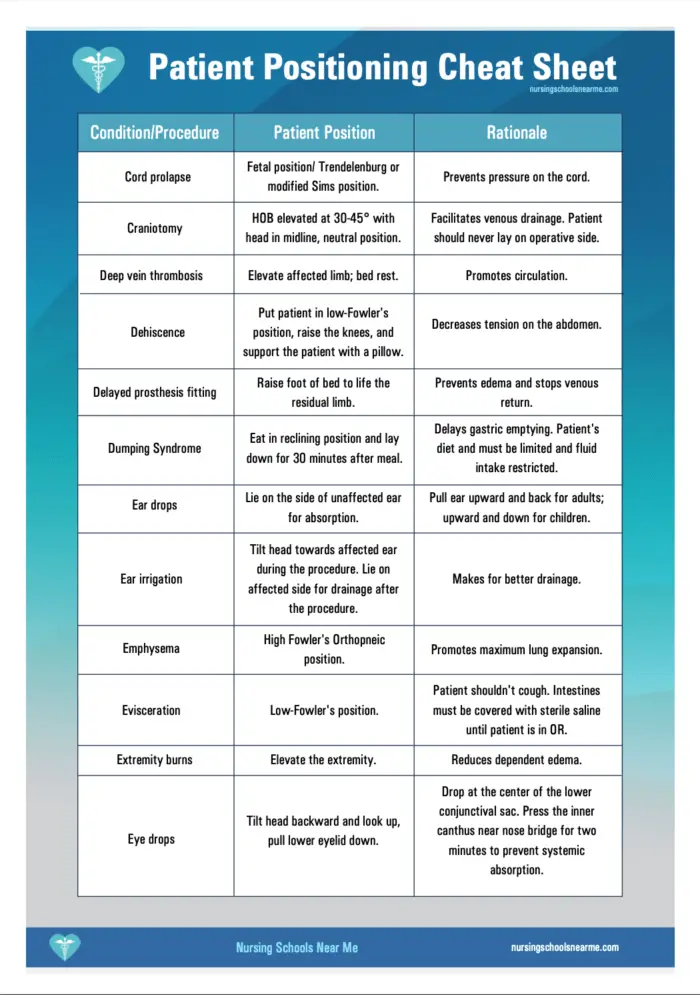
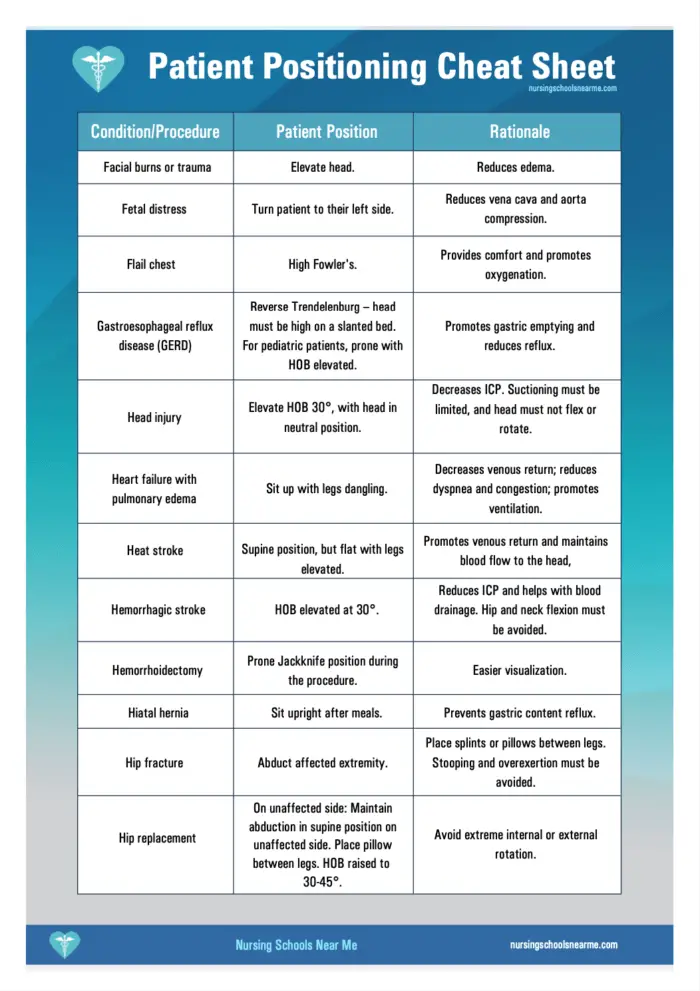
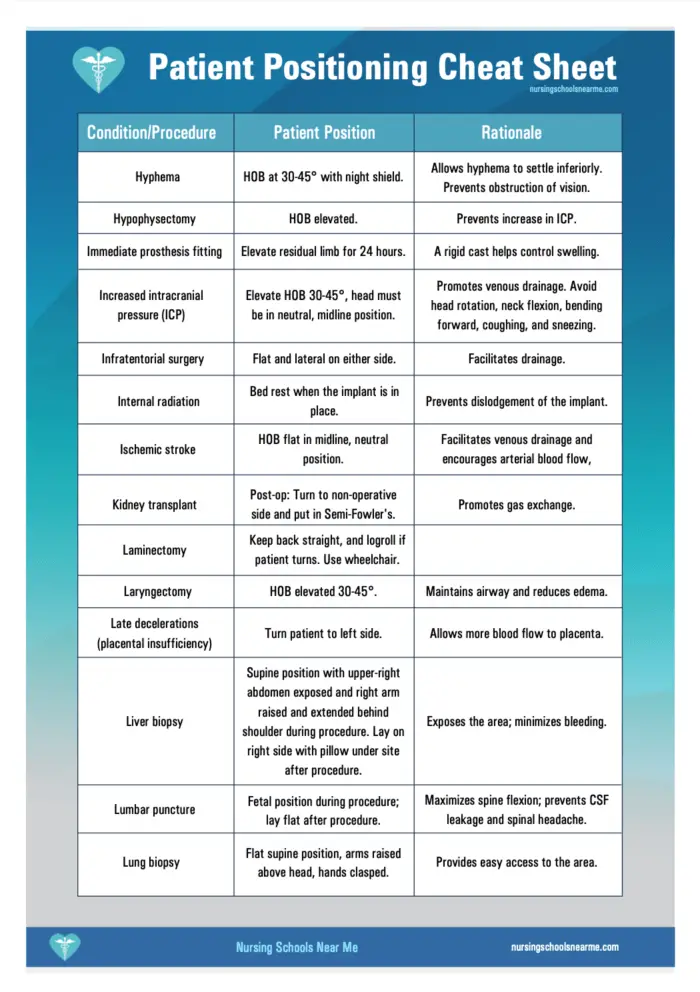
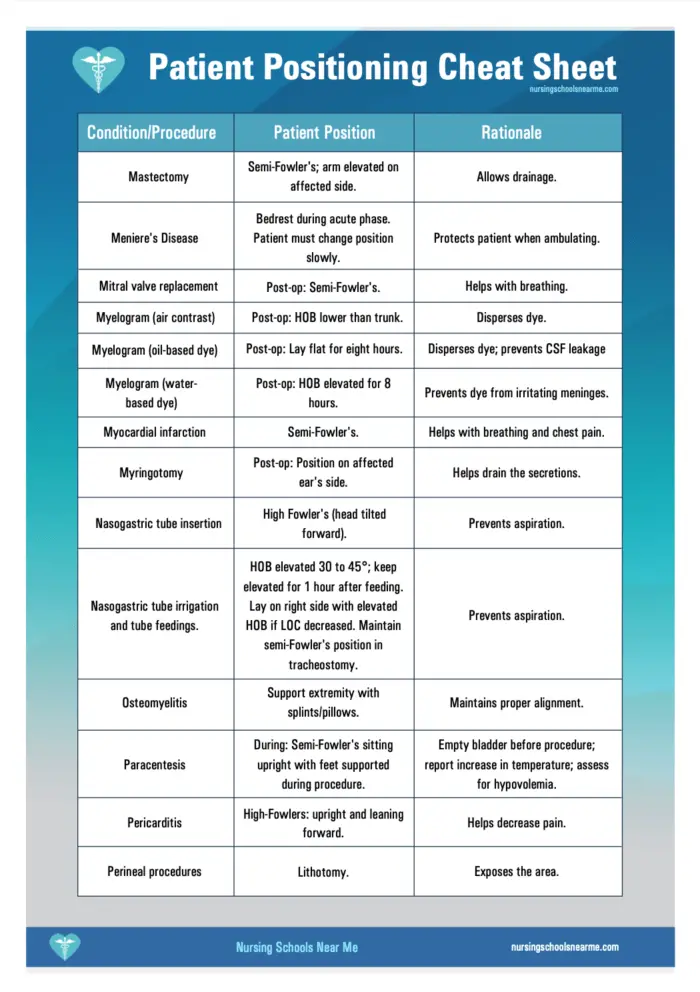
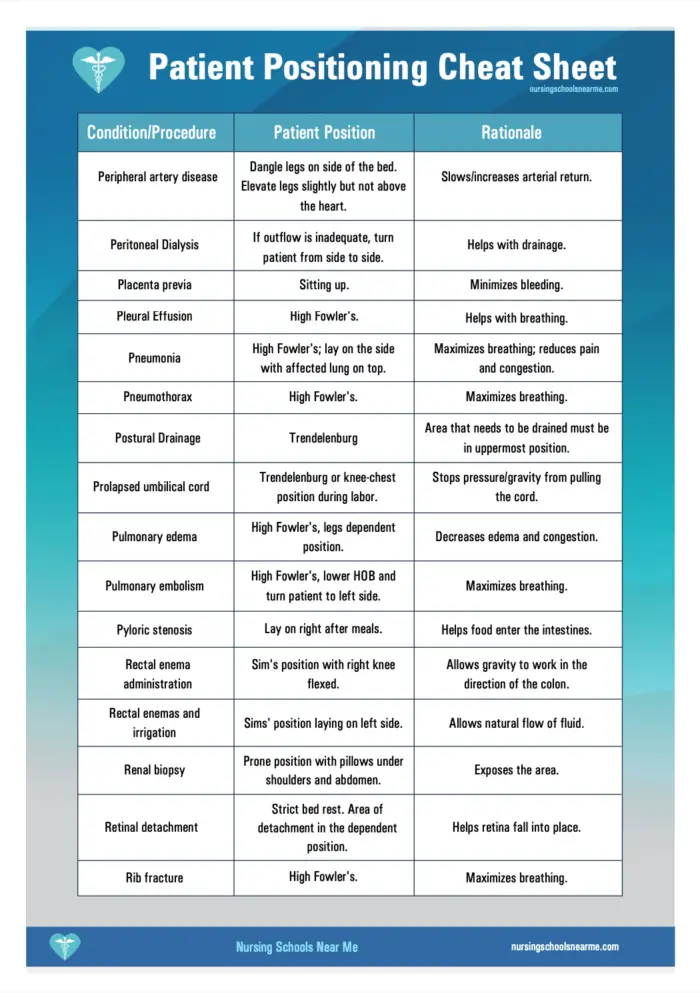
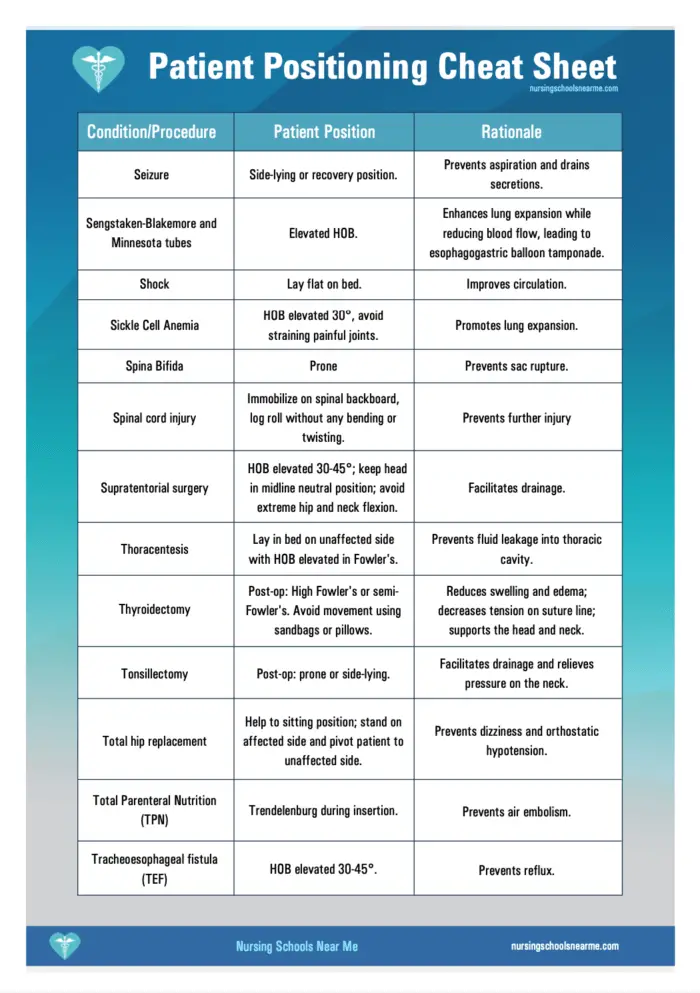
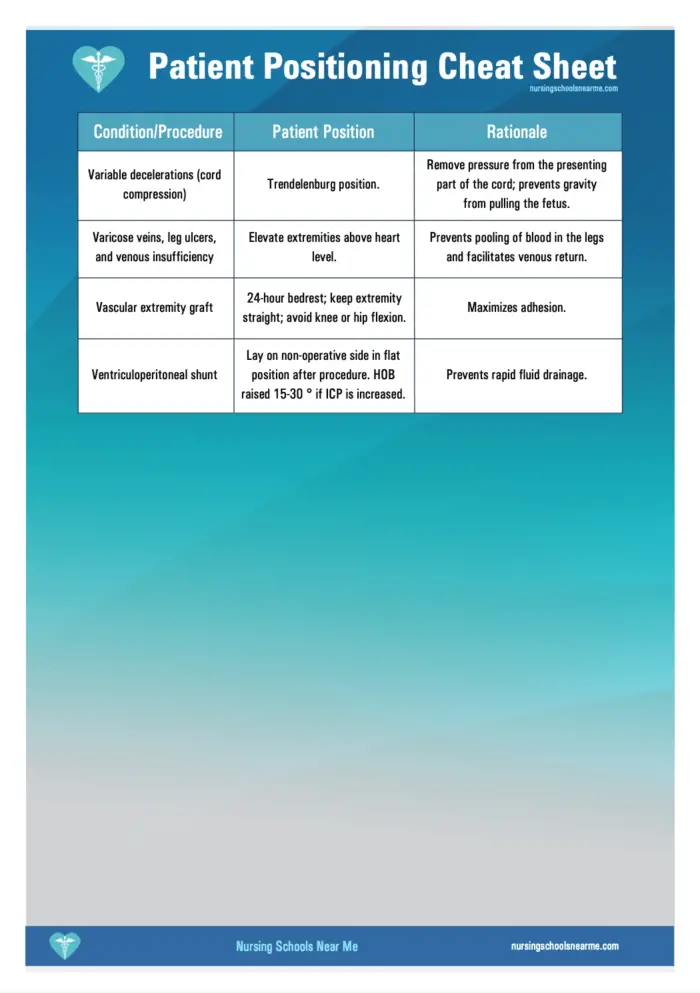
Patient Positioning Cheat Sheet
Download or print the PDF cheat sheet for patient positioning below. Or, click on the images and save them directly to your mobile device.
Simply click on each image and save.
Goals of Patient Positioning
- Ensuring patient safety and comfort. This is done by maintaining circulation, preventing unnecessary extension and rotation, and supporting the patient's airway.
- Maintaining patient dignity. A key part of proper positioning is ensuring patient dignity by avoiding or minimizing exposure.
- Allowing maximum access and visibility. Optimal positioning makes for easy surgical access and anesthetic administration.
Guidelines for Patient Positioning
Proper execution of patient positioning prevents injury for both nurses and patients. Here are the guidelines that nurses need to follow.
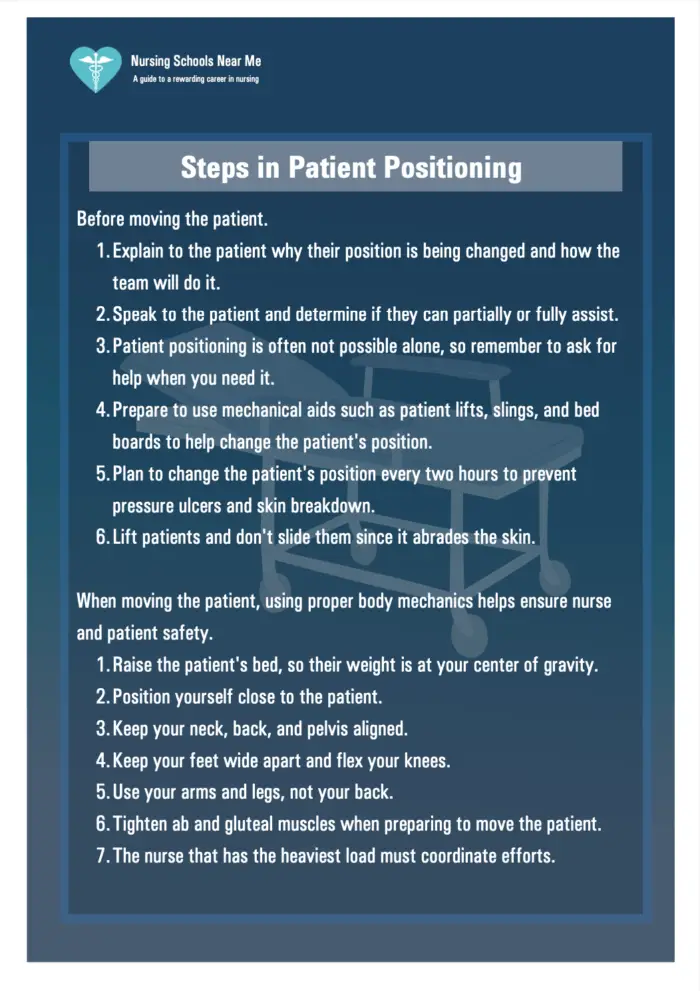
Before moving the patient.
- Explain to the patient why their position is being changed and how the team will do it.
- Speak to the patient and determine if they can partially or fully assist.
- Patient positioning is often not possible alone, so remember to ask for help when you need it.
- Prepare to use mechanical aids such as patient lifts, slings, and bed boards to help change the patient's position.
- Plan to change the patient's position every two hours to prevent pressure ulcers and skin breakdown.
- Lift patients and don't slide them since it abrades the skin.
When moving the patient, using proper body mechanics helps ensure nurse and patient safety.
- Raise the patient's bed, so their weight is at your center of gravity.
- Position yourself close to the patient.
- Keep your neck, back, and pelvis aligned.
- Keep your feet wide apart and flex your knees.
- Use your arms and legs, not your back.
- Tighten abdominal and gluteal muscles when preparing to move the patient.
- The nurse that has the heaviest load must coordinate efforts.
Supportive Devices to Help with Patient Positioning
Some devices that help with patient positioning include:
- Bed boards: These are plywood boards positioned under the mattress to maintain body alignment and provide back support.
- Foot boots: Robust plastic shoes that keep the foot flexed at the right angle.
- Hand rolls: Help keep fingers slightly flexed and thumb adducted opposite to the fingers.
- Hand-wrist splints: Help maintain proper thumb alignment.
- Pillows: They can be used to support and elevate body parts, splint incision areas, and reduce pain post-operation.
- Sandbags: These contour to the body's shape and help maintain body alignment.
- Side rails: These are bars along the sides of the bed that ensure patient safety.
- Trochanter rolls: Help prevent external rotation of the legs in the supine position.
- Wedge pillows: They are heavy-foam triangular pillows that maintain legs in abduction after a total hip replacement.
How to Document Patient Positioning
When documenting the changes in patient position, note:
- The date and time of position change
- The explanation provided to the patient
- The position that patient is placed in and the rationale
- Relevant teaching provided to the patient
- Patient response
Risk Factors of Patient Positioning
Various intrinsic and extrinsic factors can lead to pressure sores in patients. But it's more important for nurses to remember that anesthetics and muscle relaxants prevent the normal defense mechanisms from protecting the patient.
For this reason, ensuring proper patient positioning and keeping the patient's body as naturally aligned as possible is critical.
Positions by Surgical Procedure
The position that the patient must be put in depends on various factors, including the procedure type. The proper position helps ensure patient comfort and optimal access to the site.
Cardiovascular Procedures
Typically, patients are put in the supine position for cardiovascular procedures. It allows easy access to the chest cavity.
Femoral-Popliteal Procedures
Fem/Pop bypass surgery involves bypassing the arteries above and below the knee. Patients are typically put in the supine position for these procedures.
Urology/Cystoscopy/GYN Procedures
These procedures require the patient to get into some variation of the lithotomy position.
ENT/Ophthalmic Procedures
Most ophthalmic and ENT procedures call for the patient to rest supine with a headrest accessory.
Split Leg/Bariatric Procedures
These procedures require mid-line access and controls for abduction. For this reason, the patient is in lithotomy position in reverse Trendelenburg.
Kidney and Thoracic Procedures
The patient is put in a lateral position with kidney elevation with the help of a lateral positioner, straps, arm boards, and headrests.
Orthopedic Procedures
There are many different orthopedic procedures, and various positions are used depending on the type of procedure. Generally, patients are put in the supine position with traction attachments.
Shoulder Chair Procedures
Patients are put into Fowler's position for these procedures. The patient can also be seated in a shoulder chair (or “beach chair”) instead of using a surgical table.
List of Patient Positions
Here is a list detailing how common patient positions are performed and the rationale behind each.
Dorsal Decubitus or Supine Position
The supine position is where the patient lies flat on their back. Besides ENT, neck, and face procedures, the supine procedure is used in cardiac, abdominal, intracranial, laparoscopic, and endovascular procedures. It is the most common position patients are put in.
To put the patient in this position, nurses must lay the patient face-up. A pillow is used to slightly elevate the patient's head and shoulders (unless spinal anesthesia is administered). Next, the patient's arms must be tucked away on their sides and secured with arm guards. Depending upon the procedure, nurses may flex the patient's arms or extend them and secure them on padded arm boards.
Putting a patient in this procedure puts pressure on the bony prominences in areas such as the elbows and heels. Additionally, patients in this position are at increased risk of nerve damage.
Trendelenburg Position
In this position, the head of the bed (HOB) is lowered, and the foot of the bed is raised. The patient's arms are tucked at the sides, and the body is secured to the surgical table to prevent injury due to sliding.
In addition to sliding, the risks to the patient include diminished tidal volume, lung capacity, and pulmonary compliance. Putting a patient in this position can also cause venous pooling towards the patient's head. Teams must avoid putting extremely obese patients in this position for these reasons.
The Trendelenburg position might look punishing, but it is especially useful in gynecology, colorectal, and lower abdominal procedures. Additionally, it makes for easy visualization and access in central venous catheter placement, cardioversion, and genitourinary surgeries.
Reverse Trendelenburg Position
This is a common variation of the Trendelenburg position. In Reverse Trendelenburg, the head of the bed is elevated, and the foot of the bed is lowered. Since the patient must be held on a slanted bed, it is important for medical teams to use padded footboards to prevent sliding. The footboards also help reduce the risk of potential nerve injury due to ankle or foot flexion.
Besides risks to the perineal and tibial nerves, putting a patient in reverse Trendelenburg position also increases the risk of deep vein thrombosis.
Patients are put in this position for stomach, gallbladder, and prostate surgeries. It is also helpful in laparoscopic, bariatric, gynecology, and head and neck surgeries.
Fowler's Position
The patient is lying on the bed in this position, with the HOB lifted to about 45°-60°. For this reason, the position is also known as the “sitting position” and “beach chair position.”
The position puts the patient at risk of air embolism and DVT formation in the lower extremities. There is also a high risk of skin injuries from shearing and sliding.
It is essential for surgical staff to prevent the elevation of the patient's head to minimize these risks. Furthermore, the arms must be flexed and secured, the buttocks padded, and the knees flexed at a 30-degree angle.
The position offers excellent benefits in nasal surgeries, breast reduction surgeries, and nasal surgeries.
There are three varieties of this position: low Fowler's (15°-30°), semi Fowler's (30°-45°), and high Fowler's (nearly vertical).
Semi Fowler's Position
The semi Fowler's position is typically used when the patient is having difficulty breathing. Additionally, it is used during childbirth and helps with drainage during an abdominoplasty.
Since the elevation angle is smaller than the regular Fowler's position at 30 degrees, nurses may raise the bed at the knees to bend the patient's legs.
High Fowler's Position
It is the same as Folwer's position, but the head of the bed is raised to between 60 and 90 degrees relative to the lower part of the body. Nurses may leave the legs straight or bend them.
It helps elderly patients digest food and overcome breathing problems. High Fowler's is also helpful during X-rays and when patients are defecating.
Lithotomy Position
The patient lays on their back in the lithotomy position with the hips and knees flexed and thighs spread apart. Patients are conventionally placed in stirrups for their comfort and the surgical team's convenience.
The lithotomy position has four modifications: low, standard, high, and hemi. Each modification involves the patient's knees being flexed at higher and higher angles. A patient is at high risk of fracture, hip dislocation, and muscle, nerve, and pressure injuries in this placement. Since the legs are pushed against the torso in this position, the patient's lung capacity is diminished.
Patients are put in this position during childbirth or other procedures in the pelvic area. When operating, the staff must avoid leaning against the patient's inner thighs and hyperabduction of the patient's hips.
Nurses positioning the patient in this position must ensure that the patient's weight is distributed over as wide of an area as possible for maximum support.
Lateral Position
Also called the side-lying position, in the lateral position, the patient is lying on one side of their body. Their top leg is in the front, and the legs are flexed at the hip and knees. A pressure-reducing mattress or a tabletop pad must be used to minimize patient discomfort. It is also vital that a safety restraint be used across the hips and neck and spinal alignment be maintained throughout the procedure.
Taking these safety measures helps manage the risk of venous pooling, brachial plexus injury, and DVT, among others.
Patients undergoing neurosurgery, ENT, and thoracic surgeries are most commonly put in this position. However, nurses may also put patients in this position for back, hip, and colorectal surgeries.
Left and Right Lateral Positions
Depending on which side the patient is being operated on, the patient will lie on either their right or left. Positioning the patient on their left side is called the left lateral position, and when the patient lies on the right, it is called the right lateral position.
Tripod or Orthopneic Position
It is a sitting position where the HOB is elevated to 90 degrees, and the patient is seated with their back against the elevated HOB. An overbed table is then positioned in front of the patient, and pillows are piled on the table. The patient then bends forward and rests their upper body on the pillows. Nurses can also put patients in this position on the side of the bed.
The position helps patients with breathing by ensuring maximum chest expansion. Additionally, since the lower part of the chest is pressed up against the edge of the overbed table, patients in the position can exhale with ease.
Decubitus Position
The word “decubitus” means “lying down.” Therefore, any position that involves lying down is a decubitus position. There are many variations of this position, which are designated according to the part of the body touching the surface.
In the dorsal decubitus position, the back is touching the surface, and in the ventral decubitus position, the anterior is touching the surface.
Left and Right Lateral Decubitus Position
The left or right lateral decubitus positions involve the patient's left or right sides touching the surface, respectively.
Prone Position
The prone position is one of the most convenient positions for spine and neck surgeries. In this position, the patient is lying face-down on the abdomen. The head is placed in a neutral position with the help of a face positioner. It is also used in neurosurgeries, vascular surgeries, and tendon repairs.
It is important for nurses to keep the pressure off the eyes, cheeks, ears, and breasts when putting a patient in this position. Conventionally, at least four surgical staff must be available when a patient is put in the prone position.
The risks of putting patients in this position include bleeding, nerve injuries, increased abdominal pressure, ocular injuries, cardiovascular compromise, and ocular injuries.
Sims or Semiprone Position
The Sim's position involves the patient assuming a posture halfway between prone and lateral positions. For this reason, it is sometimes called the semi-prone position. It is also considered a variation of the left lateral position.
The patient is typically awake and rolls to their left side in this position. Next, the staff secures the patient to the table with body restraints. The left leg is kept straight, and the patient must slide their left hip backward and bend the right leg. This allows the surgical staff to access the anus.
The lowered arm is placed behind the patient, and the upper arm is bent at the shoulder and elbow.
Knee-Chest Position
The knee-chest position is of two kinds. The patient is on their side in the lateral knee-chest position, with the torso diagonal across the table and the hip and knees flexed.
In the prone knee-chest position, the patient kneels on the table, with the shoulders lowered onto the table. The face and the chest rest on the table.
Patients are typically put in this position for a sigmoidoscopy without administering anesthesia. It is also helpful in rectal and gynecologic exams.
Jackknife Position
It is also called the “Kraske” position. In the jackknife position, the patient lays flat on a scissored bed. For this reason, the hip is elevated, and the legs and head are lowered. The position is similar to the knee-chest position and is most commonly used for colorectal surgeries. It is also used in adrenal surgery and some back surgeries.
Putting a patient in this position can be challenging, and at least four members of the staff must be present to perform the positioning on the operating table. Patients in this position experience abdominal compression, and inferior vena cava compression also occurs. This increases the risk of deep vein thrombosis.
It is important for nurses to place extra padding at the patient's knees since the position puts heavy pressure on the knees.
Kidney Position
It is a modified lateral position where the abdomen is placed over a lift on the operating table. Since the patient is on their contralateral side, the lift bends the body, giving access to the retroperitoneal area. When patients are put in this position, a kidney rest is placed under the patient at the lift.
A pillow is placed between the legs, and the contralateral arm under the body is protected with padding. The contralateral knee is flexed, and the upper leg is kept straight to improve the patient's stability.
The Association of Operating Room Nurses (AORN) did this photo essay on safe patient positioning that you may find useful.