PR Interval: A Comprehensive Guide
The PR interval in a heartbeat illustrates the delay in the conduction of the AV node. However, there's a lot more to PR intervals than just that.
To understand PR intervals, you must learn to read an ECG. Learning to read an ECG takes a lot of practice, and you will only fully get it when you look through hundreds of 12-lead ECG tracings.
In this post, we break down what PR intervals are, what causes long and short PR intervals, and how a nurse can diagnose and manage the underlying problem. Most importantly, we cover how to read an ECG so you know how to identify various PR intervals.
What is the PR Interval?
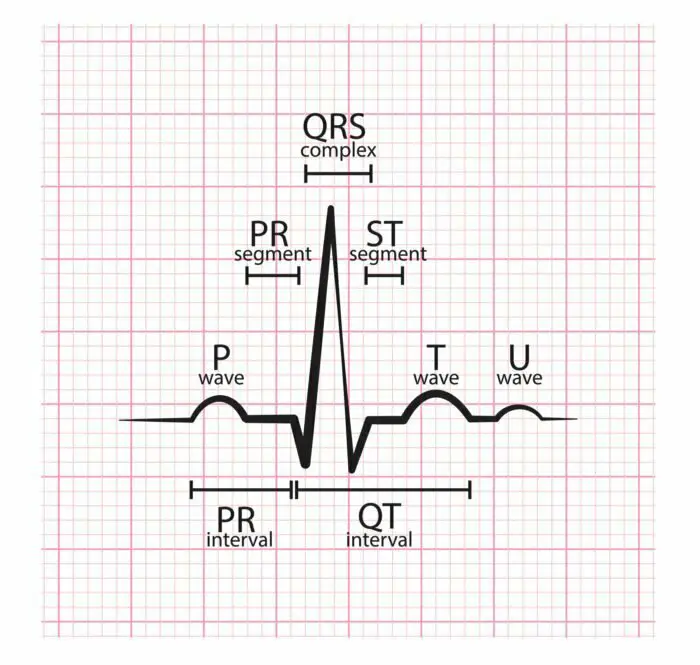
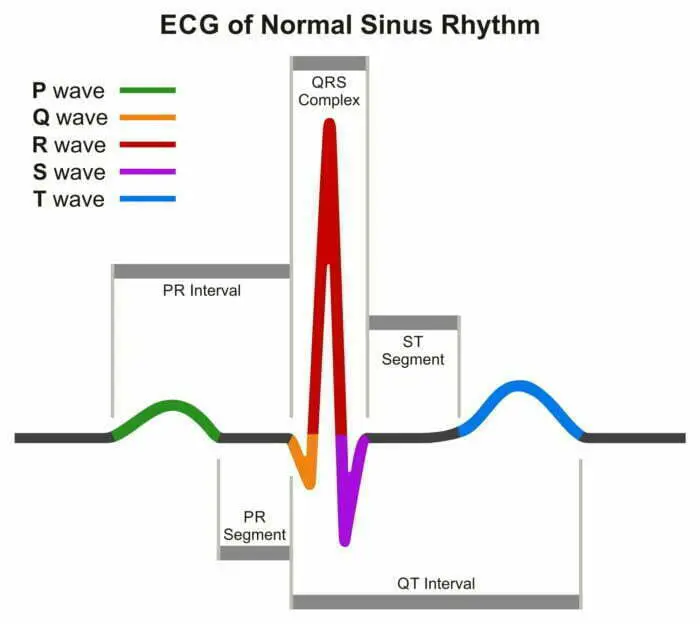
The PR interval is the period between the beginning of the P-wave (representing atrial depolarization) and the beginning of a QRS complex (representing ventricular depolarization), and it indicates conduction through the AV node.
The PR interval illustrates the time it takes for the sinus node to generate an electrical impulse, travel through the atria, across the AV node, and to the ventricles of the heart.
Normal PR Interval
A normal PR interval typically takes between 0.12 and 0.20 seconds – three to five small squares on the ECG). This period is considered the normal PR interval. An abnormal PR interval can indicate many things in a patient. But before you learn about the causes, you must learn that an abnormal PR interval can be prolonged or shortened.
Prolonged PR Interval
PR interval is said to be prolonged when there is delayed conduction through the AV node. However, the delayed conduction may be present in other sites in the heart. Prolonged PR interval can occur independently or alongside other heart blocks, such as a second-degree AV block.
Traditionally, a prolonged PR interval (PR interval longer than 200 ms) has been called a “first degree AV block.” That said, “delayed AV conduction” is a more appropriate way to refer to the condition.
It's important to note that a PR interval has the potential of being altered by changing sympathetic and parasympathetic tones. This is why certain medications, such as beta-blockers, often lengthen the PR interval and cause a first-degree atrioventricular block.
A prolonged PR interval causes the first heart sound to sound soft during an examination.
Shortened PR Interval
The shortened PR interval is typically seen when the AV node delay is bypassed. This typically happens in patients with Wolff-Parkinson-White syndrome or Lown-Ganong-Levine syndrome.
Any PR interval shorter than 120 ms is considered a shortened PR interval. If a patient has a shortened PR interval, it can cause the first heart sound to sound louder. We discuss the causes of a shortened PR interval in detail in later sections.
How to Read an ECG
You can use several different ECG interpretation systems to interpret a 12-lead ECG. Here's a system that will help you ensure that you never miss any important details:
#1 Determine Details of the Patient
The first thing you should look at is the patient's name and date of birth. If you're a nurse in the emergency department, chances are, you will need to review several ECGs at once.
EKG Interpretation Cheat Sheet
Learning the location of every patient will help you decide if a patient must be moved to a higher dependency area.
#2 Learn Details of the Circumstances
It's critical for any healthcare professional reading an ECG to understand the patient's circumstances. Make sure you get answers to all of the following questions:
- At what time was the ECG done?
- How many ECGs were done?
- Was the patient experiencing chest pain at the time of the ECG?
—
Note: It's natural to be concerned about the dynamic changes in the ECG. Understanding whether several ECGs were done will help you determine if it's a serial ECG exam report. If it is, the report will typically have three ECG reports that you can compare for a clearer idea of the patient's condition.
—
#3 Measure the Rate on the ECG
After you've collected all of the essential information you'll need to make an assessment, you should measure the rate of the ECG. You can do this in two ways:
- Count the number of QRSs on one line (typically running along the bottom of lead II), and multiply the number with six.
- Count the number of large squares between the R waves and divide the number by 300.
Remember that reporting a rate range instead of a single number is the better way to go if your patient is in atrial fibrillation.
#4 Assess the Rhythm on the ECG
The next steps involve assessing the heart's rhythm using the ECG. Ask yourself if the heart's rhythm is regular or irregular? Is it regularly irregular or irregularly irregular?
The heart's rhythm can be challenging to assess in tachycardia and bradycardia. However, doing a paper test can make finding the pattern easier.
To do a paper test, grab a scrap piece of paper, and place it over the ECG. Pick any QRS complex, and mark a dot on top of it. Draw another dot on top of the next QRS complex, and slide the paper along the ECG.
If the two dots match the tops of the QRS complexes throughout the ECG, the rhythm is regular. Else, the rhythm is irregular.
#5 Assess the Axis on ECG
The axis on an ECG is the sum of the heart's electrical activity. You need to remember that the contraction travels from the atria to the right and left ventricles. Since the left ventricle is much larger and muscular, a normal axis lies between 30 and 90 degrees.
Typically, if the net deflections in lead I and aVF are positive, the axis is normal. However, there may be deviations in the axis, which is something you should look out for.
If lead I depicts a negative deflection and the aVF has a positive deflection, the axis deviates to the right. In contrast, the axis deviates to the left if lead I has a positive deflection, and the aVF has a negative deflection.
While this general method is accurate enough to help you assess the axis, there is a way to assess it in more detail:
First, in aVF, you must count the number of squares that have positive or negative deflection. Next, make a dot on the aVF axis, moving a millimeter up or down depending on the polarity of the deflection. For a positive deflection, move a millimeter upwards, and for a negative deflection, move a millimeter downwards.
Next, count the small squares with a positive and negative deflection on lead I. Make a dot on the lead I axis, moving according to the polarity of the deflection. For a positive deflection, move a millimeter to the left, and for a negative deflection, move one millimeter to the right.
Draw a horizontal line through the dot on the lead I axis and a vertical line through the dot on the aVF axis. The lines will meet at some point, and you must draw a line from the intersection to the 0. This will give you an accurate axis.
Causes of Axis Deviation
The axis can deviate for many reasons.
Left Axis Deviation
- Left anterior fascicular block
- Left bundle branch block
- Left ventricular hypertrophy
- Inferior MI
- Ventricular ectopy
- Paced rhythm
- Wolff-Parkinson White syndrome
Right Axis Deviation
- Normal if the diaphragms are raised due to pregnancy or Ascites
- Normal in children and thin young adults
- Hyperkalaemia
- Often caused due to respiratory disease
- Ventricular tachycardia
- Septal defect
- Left ventricular hypertrophy
- Right ventricular hypertrophy
- Paced rhythm
- Pulmonary embolism (PE)
- Left anterior hemiblock
- Left posterior hemiblock (this is rare)
- Inferior myocardial infarction
- Anterolateral myocardial infarction
#6 Assess P-wave and PR interval
You must check if there is a P-wave. Often, in atrial fibrillation, atrial flutter, and junctional tachycardia, P-waves are not visible.
If you find P-wave, you must determine if the waves are associated with QRS complexes. A P-wave is not associated with a QRS complex indicates a complete heart block.
After you determine whether there is a P-wave or not, you must assess the morphology. You may find that P-waves have notches. These P-waves are called “P mitrales” and indicate that the heart has Left Atrial Hypertrophy. This LAH is typically caused by mitral stenosis.
In other cases, you may find that the P-waves have tall peaks. These are “P-pulmonales” and indicate Right Atrial Enlargement or Right Atrial Hypertrophy. The RAH is often a result of pulmonary hypertension or tricuspid stenosis. Hyperkalemia also sometimes causes P-pulmonales.
You must also assess the PR interval at this point. A prolonged PR interval often indicates a first-degree atrioventricular block.
On the other hand, the PR interval is typically shorter if there is rapid conduction via accessory pathways, such as in the Wolff Parkinson White syndrome. If you notice depression in PR intervals, it may indicate pericarditis.
#7 Assess the Q-Wave and QRS Complex
The Q-wave is the downward deflection in the initial part of a QRS complex. You will find that these deflections are normal in the leads on the left side of the chest (V5, 6, leadI, and aVL). This is because these specific deflections represent the septal depolarization from left to right.
However, this representation is only accurate as long as the Q-wave is shorter than one small square (meaning <0.04 seconds long) and less than <2mm deep. If you see that the Q-waves are larger than that on any other ECG leads, you can be sure they are pathological.
A normal QRS complex is no longer than three small squares (or <0.12 seconds). A wide QRS complex can be a result of:
- Hyperkalaemia
- Tricyclic antidepressant (TCA) poisoning
- Bundle branch blocks
- Ventricular pre-excitation due to conditions like WPW
- Ventricular rhythm
- Paced rhythm
It is also vital for you to assess the shape and height of the QRS complex. If the QRS complex is small, it may be due to a high BMI, pericardial effusion, cardiac amyloid, emphysema, or cardiomyopathy.
If the height of the R wave in V6 added to the depth of the S wave in V1 is higher than 35mm, the QRS is tall, indicating left ventricular hypertrophy. You must remember that the QRS complex tends to be tall in children and thin young adults.
#8 Assess ST Segment
ST segments in ECG can be normal, depressed, or elevated. You must assess whether the segment is depressed or elevated by one or more millimeters in two limb leads in a row. You must also determine if the segment is elevated or depressed by two or more millimeters in two consecutive chest leads. Keep an eye out for reciprocal changes as well.
If you notice ST elevation, it is an indicator of infarction. If you notice ST depression, it may be due to ischemia. Digoxin toxicity also causes ST depression and is indicated by a downsloping ST depression.
Benign early repolarization or “high-takeoff” mimics ST elevation, which should be kept in mind. A high-takeoff has a concave ST elevation and typically has a slurry j-point. It most prominently appears in leads V2 through V5. It is benign, and you will see a high-takeoff in young people.
It's essential to differentiate between a high-takeoff and a myocardial infarction. In addition to having the traits mentioned above, a high-takeoff will also have the following traits:
- The ST elevation is minimal compared to the amplitude of the t-wave
- The ST segments don't change over time
- There are no reciprocal changes
#9 Assess QT Interval
A QT interval is the period between the beginning of the Q-wave and the end of a T-wave. It's corrected for the heart rate, and the corrected value is called QTc.
You can quickly check if the QT interval is normal by determining if the T-waves are about halfway between the QRS complexes. If the T-waves are over halfway between the QRS complexes, it typically indicates that the QTc is lengthened. This isn't a very accurate way of checking the QT interval, but it is fast and convenient.
Healthcare workers need to identify long QTc intervals in patients with a history of collapse.
A prolonged QT has several causes: from the effects of drugs and TCAs to conditions such as hypocalcemia and myocarditis.
#10 Assess T-wave
A T-wave can be inverted or flattened due to ischemia, ventricular hypertrophy, LBBB, digoxin toxicity, and hypokalemia. It's also important to note that hyperkalemia typically causes t-waves to be peaked. In the case of hyperkalemia, the ECG will also have a small p-wave and wide QRS complexes, which indicates severe cardiac toxicity.
What is the Heart Block Poem?
The heart block poem is:
If the R is far from the P, then you have a First Degree.
If PR gets longer and longer before the QRS drop, it must be a Wenckebach.
If PR stays normal and QRS quits, it must be a Type II Mobitz.
If Ps and Qs beat independently, it must be a Third Degree.
We will use the heart block poem below to help remember each type of block.
Atrioventricular Heart Blocks
Atrioventricular blocks are conduction defects that impair the conduction of atrial impulses to ventricular pathways. These are three types of AV heart blocks and two sub-types of the second degree heart block.
First Degree AV Block
Catchphrase: First-Degree = Far away P
Poem: If the R is far from the P, then you have a first degree.
A first degree atrioventricular block displays the following characteristics:
- Heart rate between 60 and 100 BPM
- Prolonged PR interval
- Normal QRS complex
- Regular heart rhythm
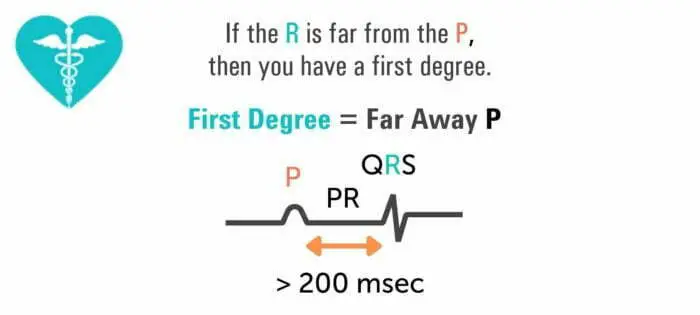
The causes of a first-degree AV block include:
- Hyperkalemia
- Hypokalemia
- Inferior wall MI or ischemia
- Calcium channel blockers or digoxin toxicity
- Use of antidysrhythmics and amiodarone
It is an asymptomatic arrhythmia and must be treated by finding and treating the underlying cause. If healthcare workers detect the development of symptomatic bradycardia, or the PR interval is longer than 0.26 seconds, they must administer atropine.
Second Degree AV Block
Mobitz I or Type I Wenckebach
Catchphrase: Wenckebach = Longer Before Drop
Poem: If PR gets longer and longer before the QRS drop, it must be a Wenckebach.
To detect a second degree AV block, look for the following details in an ECG report:
- Regular atrial rhythm
- Irregular ventricular rhythm
- Atrial rate faster than the ventricular rate
- Progressively and slightly longer PR intervals until the QRS complex disappears
- Shorter PR interval after dropped heartbeat
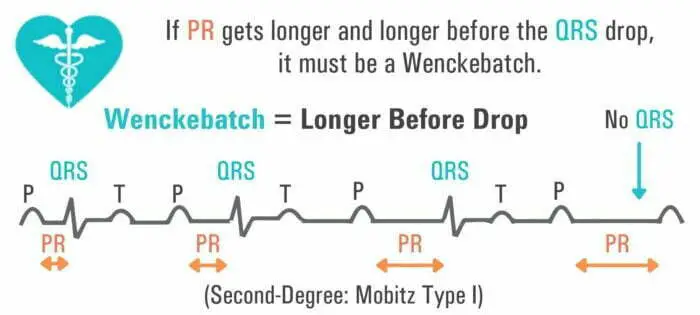
A second-degree AV block is asymptomatic; however, it does have clinical manifestations. The patient may complain of weakness and vertigo and have an irregular pulse.
The condition is caused due to inferior wall MI and acute rheumatic fever. However, it can also appear after heart surgery and vagal stimulation. It is usually treated by treating the root cause, but atropine may be administered for management.
If symptomatic bradycardia appears, cardiologists can recommend implanting a temporary pacemaker. If appropriate, digoxin must be discontinued.
Second Degree AV Block Mobitz II
Catchphrase: Mobitz = QRS Quits
Poem: If PR stays normal but QRS quits, then it must be a Type II Mobitz.
A second-degree AV block Mobitz II has the same clinical manifestations as second-degree AV block Mobitz I. However, its characteristics on an ECG report are different:
- Regular atrial rhythm
- The ventricular rhythm may be regular or irregular, depending on the degree of the block
- Constant P-P interval
- QRS complex disappears or is periodically absent
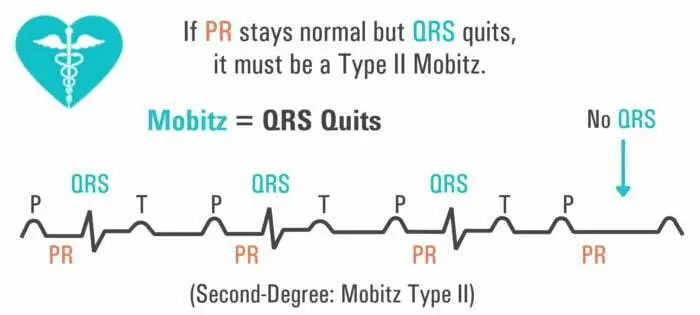
The condition is caused by acute myocarditis, digoxin toxicity, anterior wall MI, or severe coronary artery disease.
Appropriate drugs such as epinephrine or dopamine may be administered if symptomatic bradycardia develops. A pacemaker may be installed if required. Digoxin must be discontinued if appropriate.
Third Degree AV Block
Catchphrase: Third-Degree = Beat Independently
Poem: If Ps and Qs beat independently, it must be a third degree.
Also called a complete heart block, its characteristics on an ECG include:
- Regular atrial rhythm
- Regular ventricular rhythm (but slower than atrial rate)
- PR interval irregular
- P waves and QRS complexes have no relation
- QRS interval may be regular or abnormally wide and peculiar
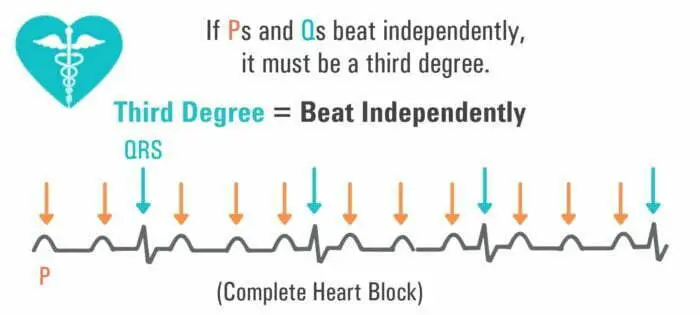
The arrhythmia clinically manifests as heart failure, hypotension, and angina. The possible causes include congenital abnormalities, digoxin toxicity, hypoxia, MI, rheumatic fever, and Lev's disease.
A pacemaker can help manage the condition, but nurses may administer dopamine or epinephrine if bradycardia occurs.
Causes of Short PR Interval
A short PR interval appears if the patient has preexcitation syndromes or has an AV nodal rhythm.
Wolff-Parkinson-White Syndrome and Atrial Fibrillation
The WPW syndrome is a preexcitation syndrome in which the ECG has a PR interval shorter than 120 ms and a wide QRS complex. Furthermore, the QRS complex has a slurred upstroke.
The condition occurs in patients who have a bypass tract that connects the electrical system of the atria to the ventricles directly.
In a healthy heart, the action potential of the sinus node always passes through the AV node to get to the ventricles.
But in patients with WPW, the accessory pathway enables conduction to skip passing through the AV node. This also causes the ventricles to get depolarized quickly. The pre-excitation of the ventricles causes a shorter PR interval.
Patients can have WPW and atrial fibrillation together, and the combination is potentially fatal, particularly if AV blocking agents are administered.
Patients with both conditions display erratic atrial action potentials between 400 and 600 BPM conducted through the bypass tract extremely fast. For this reason, patients with WPW that develop atrial fibrillation have much higher ventricular rates than patients with atrial fibrillation but without WPW.
Administering AV blocking agents reduces the number of action potentials that pass through the AV node and increases the impulses going through the bypass tract. In this way, the ventricular rate increases, causing ventricular fibrillation and death.
Patients with both conditions must be administered procainamide. However, electrical cardioversion is also an option, given the patient is hemodynamically unstable.
Lown-Ganong-Levine Syndrome
Patients with the LGL syndrome have a short PR interval in the ECG, along with regular P waves and QRS complexes. Delta waves are absent in the ECG.
The syndrome occurs in patients with a congenital bypass tract connecting the atria and the ventricles. The accessory pathway enables the heart to bypass the AV node in the same way that WPW syndrome does.
For this reason, when the sinus node fires, the action potential does not pass through the AV node like it typically does. Instead, the impulse travels down the bypass tract and activates the ventricles a lot faster than normal. The shortened duration of the sinus node firing and the depolarization of ventricles results in a short PR interval.
There is a key distinction between the WPW and the LGL syndrome. In the WPW syndrome, the bypass tract connects to the ventricular myocardium. But in the LGL syndrome, the bypass tract connects to the normal conduction pathway distally.
This results in both conditions causing a short PR interval. However, in the ECG of an LGL syndrome patient, the QRS complex will not be wide, and a delta wave will not be present. This is because the ventricular activation is normal in the LGL syndrome, but in the WPW syndrome, it occurs from myocyte to myocyte.
A similar arrhythmia typically occurs alongside both LGL and WPW syndromes, including AVRT and rapid atrial fibrillation. But the treatment of both the conditions is similar, with procainamide being most frequently utilized.
That said, ablation of the bypass tract is more challenging in patients with LGL syndrome since the accessory pathway is much closer to the AV node. Ablation poses a high risk of a complete heart block, which necessitates the implantation of a permanent pacemaker.
AV Nodal Rhythm/Junctional Rhythm
Junctional rhythms are regular rhythms with a narrow complex that arises from the AV node. These typically don't have P waves, and if they do, they are abnormal. The PR interval is short.
The AV nodal rhythm occurs when the heart's electrical activation occurs within or near the AV node. In a regular healthy heart, the electrical activation comes from the sinoatrial node.
Since the His-Purkinje system is used, the QRS complexes tend to be narrow. It's further necessary to note that a junctional rhythm is typically slower than 60 BPM. However, it is called an accelerated junctional rhythm when it is fast.
The origin point of electrical activation makes it rare for a P wave to appear. It is typically buried in the QRS complex or appears slightly after the QRS complex ends.
It's also important to note that the morphology of the P wave in junctional rhythm is not similar to the sinus P wave. Sinus P waves are typically biphasic in lead V1 and upright in lead II. However, in patients with this condition, the P wave is inverted in lead II, if it is visible at all.
If the cause of the condition is not reversible, a pacemaker may be installed to relieve the symptoms.
Conduction Through the His-Purkinje System
Besides the physiologic possibilities, alterations in the PR interval sometimes represent an abnormal progression of electrical conduction from the atria to the ventricles via the AV node.
These manifest as PR interval prolongation or shortening.
Differential Diagnosis for Shortened and Prolonged PR Interval
The first step to determining the differential for an abnormal PR interval begins by excluding the abnormality considering normal PR variability. After this is done, a diagnostic algorithm is used based on the length of the PR interval.
Normal PR Variability
The PR interval can vary with the heart rate in a normal physiologic state. This is caused by the variations in sympathetic tone.
An increased tone makes for increased conduction at a faster heart rate. In contrast, the withdrawal of the sympathetic tone slows conduction.
But regardless of these variations in physiology, a normal PR interval lies between 140 ms and 200 ms. Young adults and athletes sometimes have a PR interval longer than 200 ms for physiologic reasons.
Administering atropine shortens the PR interval; however, this doesn't work for patients with an underlying pathophysiologic cardiac disease.
PR Interval < 0.12 s
If the PR interval is shorter than 120 ms, the diagnosis is limited mainly to the existence of a bypass tract between the ventricles and the atria. The PR interval tends to be shorter since the cardiac current bypasses the AV node and travels directly between the ventricles and atria (WPW).
However, the bypass tract may also exist between the AV node and the atria.
PR Interval > 0.2 s
Typically, patients that have isolated instances of prolonged PR intervals are asymptomatic. That said, prolonged PR intervals are sometimes associated with a high-grade AV block. In this case, the patient may experience symptoms such as fatigue, frank syncope, and decreased exercise tolerance.
Patients whose ECGs have a prolonged PR interval tend to be older with a history of cardiovascular disease. That said, young adults and athletes sometimes have asymptomatic PR prolongation.
To sum up, a prolonged PR interval can be caused by a first-degree heart block or second-degree heart block of Mobitz Type I or Mobitz Type II.
Diagnostic Approach to PR Intervals
Diagnostic Approach to Shortened PR
Learning the patient's history in detail can help differentiate between shortened PR interval due to physiological reasons and shortened PR interval due to accelerated conduction via an accessory pathway.
Typically, patients with a physiologic problem get clinical attention because of an ECG. They aren't symptomatic. Knowing this, a patient that has a short PR interval and reports a history of sudden palpitations must be considered as having a physiological problem during diagnosis.
It's important to note that patients with bypass tracts are sometimes asymptomatic. So you cannot remove the possibility of a bypass tract if a patient lacks symptoms and a short PR interval.
Besides learning the patient's history, examining the ECG closely can help ensure an appropriate diagnosis.
Diagnostic Approach to Prolonged PR
To diagnose a prolonged PR with ECG analysis, you must determine the severity of the AV node dysfunction. There may be a delay in conduction, or a complete lack of conduction in the AV node, indicating a complete heart block.
A prolonged PR is often associated with other abnormalities, so you need to examine the ECG closely.
To ensure accurate analysis, answer the following questions when you examine the ECG:
- Are the PR intervals prolonged uniformly before every QRS complex? (If yes, the patient may have first degree AV block)
- Is the PR interval irregularly irregular and gets prolonged progressively until there is no P wave at all before the QRS complex? (If yes, the patient may have a Mobitz Type I block)
- Is the PR interval shorter after the dropped beat compared to the PR interval before the dropped beat? (If yes, it's an indicator of Mobitz I)
- Are the QRS complexes clustered together? (If yes, it's an indicator of Mobitz I)
- Do non-conducted P waves appear after PR intervals? (It's an indicator of Mobitz II, typically with an intranodal block)
- Are there any pathological Q waves?
- Do the changes on the ECG suggest ischemia? (inferior wall MI in case of Mobitz I, anterior wall MI incase of Mobitz II)
It's important to remember that you can also determine the differential by looking into the etiology of the prolonged PR. The condition can result from:
- Underlying cardiac disease
- Effects of medication
- Electrolyte imbalances
- Active ischemia
- Hypothyroidism
- High vagal tone
It can also be idiopathic.
Relevant Historical Information Required for Diagnosis
For Shortened PR Intervals
Some patients that have a short PR interval due to an accessory pathway have paroxysmal supraventricular tachycardia. For this reason, it's essential to ask specific questions when enquiring about the patient's history.
You must find out if they have a history of lightheadedness, near loss of consciousness, or palpitations. You must also find out if their family has a history of syncope or unexpected cardiac death.
For Prolonged PR Intervals
When asking the patient about their medical history, you must determine whether the prolonged PR interval is associated with a higher grade heart block. Often, the conduction delay can be long enough to impair the heart's output low enough to cause lightheadedness or syncope.
You must also ask questions to find possible etiologies of their disease. Some helpful questions to ask include:
- What medications do you take? Did you recently start or stop taking any medication?
- Have you ever lost consciousness or felt as if you would faint? When?
- Do you ever feel dizzy for no apparent reason and suddenly?
- Has a doctor ever told you that you have a cardiac disease? Have you had an MI in the past?
Helpful Physical Examination Maneuvers for Accurate Diagnosis
For Shortened PR Interval
If you suspect that a patient has a bypass tract, you must request a complete cardiac exam. Patients with an accessory pathway typically do not have another cardiac abnormality. However, a bypass tract is associated with congenital heart disease, mitral valve prolapse, and heritable cardiomyopathies in some rare cases.
For Prolonged PR Interval
If a patient has a prolonged PR interval, they must get a complete cardiac exam emphasizing the pulse. The pulse could be irregular and have dropped beats (Mobitz I) or irregular with beats dropping occasionally (Mobitz I).
A complete cardiac exam will also make it easier to determine if the patient has a co-existing cardiac disease like cardiomyopathy.
Helpful Radiographic and Lab Tests for Accurate Diagnosis
For Shortened PR Interval
Depending upon the scenario, genetic testing may be a reliable way to diagnose an inherited form of WPW. This is because lab testing is generally not helpful in diagnosing a bypass tract.
For Prolonged PR Interval
Prolonged PR intervals are easy to diagnose by looking at the ECG and combining it with the etiology from the patient's history. If you determine that the longer PR interval results from medication or severe hypothyroidism, you may be able to determine the etiology via lab testing. The digitalis and TSH levels are useful indicators in these circumstances.
It's important to note that there is no such thing as a “wasted” diagnostic test when it comes to evaluating a prolonged PR interval.
Relevant Diagnosis Criteria
Diagnosis of Shortened PR
Diagnosing a bypass tract is not possible by simply looking at the ECG results. The findings could be intermittent or represent a physiological variant of the problem consistent with the enhanced AV conduction.
That said, WPW is sometimes also associated with a broader QRS complex and a delta wave. If you suspect that a patient may have a bypass tract, you should refer them to a cardiac electrophysiologist for a detailed evaluation.
Diagnosis of Prolonged PR
If the PR interval is longer than 200 ms, the interval is prolonged. You can differentiate between the various causes bearing the following characteristics in mind:
- First-degree AV block: The PR interval is prolonged uniformly before every QRS complex.
- Second-degree AV block (Mobitz I): The PR interval is gradually longer until the conduction fails. After the dropped QRS, the next PR is shortened. Group beating is another indicator of this condition.
- Third-degree AV block (Mobitz II): The PR interval has a fixed but prolonged duration, and P waves abruptly appear without the subsequent QRS appearing.
Management of Abnormal PR Interval
Management of Shortened PR Interval
Acute
A patient with a bypass tract may have supraventricular tachycardia. In patients that suffer from atrioventricular reentrant tachycardia during atrial fibrillation, the ventricles can get excited ahead of time. This increases the risk of ventricular fibrillation.
For this reason, patients with history or evidence of pre-excitation should not be administered nodal agents. Attempting to control their heart rate by this means can make their arrhythmia worse and is often fatal.
Chronic
Those with a short PR interval can be diagnosed solely with the ECG report. That said, the emphasis must be placed on assessing whether the patient has any associated symptomatic tachycardia that indicates the existence of an accessory pathway.
If a patient has symptomatic tachycardias, they must see a cardiologist quickly so they can evaluate their condition correctly and suggest treatment options. Depending on the circumstance, the cardiologist may recommend getting radiofrequency ablation.
The risk of sudden cardiac death in patients with an accessory pathway having an asymptomatic tachycardia is low. However, the risks aren't the same for every patient. Only a cardiologist can evaluate the risk and suggest the right option.
Management of Prolonged PR Interval
The management practices of a prolonged PR depend on the degree of heart blockage. In a first-degree heart block, typically, no interventions are made.
Second-degree heart block typically develops due to reversible causes. In emergencies, the management approach aims to increase the heart rate without affecting the underlying cause. In the case of a Mobitz I block, if the Heart Rate is higher than 40 and the patient doesn't have any symptoms, intervention is not necessary.
On the other hand, if the HR is lower than 40 and the patient has symptoms, 0.5 mg Atropine is typically administered. Up to three doses are given in the interval of three to five minutes, so the heart conducts more impulses through the AV node.
If the symptomatic patient is experiencing a heart block due to a reversible cause, a temporary pacemaker may be implanted until the reversible cause is addressed. A permanent pacemaker may be implanted in patients with irreversible causes.
A Mobitz II block is more likely to appear due to an irreversible cause. While the emergency management options for this kind of block are the same as the options for a Mobitz I block, Mobitz II blocks have a higher chance of developing into complete heart blocks. For this reason, patients typically require the insertion of a permanent pacemaker.
Significance of Prolonged PR Interval in the General Population
Many studies have been done on the subject of the long-term effects of a prolonged PR interval. Different studies draw different conclusions.
In a 2009 study, researchers aimed to determine the clinical significance of the prolongation of PR interval in ambulatory individuals. They studied 7575 individuals from a cohort in Framingham in Massachusetts. The mean age of the group was 46 years, and 54% of the cohort comprised women.
These individuals got a routine 12-lead ECG exam, and the cohort followed up from baseline exams in 1968 – 1974 later in 2007.
The researchers used proportional hazards models adjusted for multiple variables to determine the relation between PR interval and arrhythmic events and death. The study's outcomes included atrial fibrillation (AF), all-cause mortality, and pacemaker implantation.
When the researchers followed up with the participants of the study, 481 developed atrial fibrillation, 124 needed a pacemaker implanted, and 1739 participants died.
With that data, the researchers concluded that prolonged PR interval could be associated with an increased risk of pacemaker implantation, AF, and death.
Another study in 2013 aimed to elucidate the prognostic importance of a prolonged PR interval in the middle-aged population. The researchers investigated the first-degree AV block because of the increase in studies suggesting increased mortality and morbidity in patients with a prolonged PR interval.
The researchers evaluated the 12-lead ECG reports of 10785 patients between the age of 30 and 59. The mean age was 44 years, and 52% of the reports were of males. The data was recorded between 1966 and 1972, and the researchers followed up with the patients for 30 ± 11 years.
A PR interval longer than 200 ms was considered a prolonged PR interval; however, the researchers performed further analysis on PR greater than 220 ms.
The study's endpoints included cardiovascular mortality, all-cause mortality, hospitalizations due to heart issues, and sudden cardiac death.
2.1% of the patients had a PR interval longer than 200 ms in the baseline exam. However, the value normalized to less than 200 ms in 30% of the subject in the follow-up. There was no increase in hospitalization due to prolonged PR intervals due to heart failure, AF, coronary artery disease, and stroke.
The study concluded that the prolonged PR interval normalizes in a significant chunk of the subjects over the years they get treatment. For this reason, per this study, long PR intervals cannot be associated with an increased risk of mortality.
PR Interval Outcomes in Older Adults
The PR interval increases with age, but the progression differs by race. It is associated with endpoints such as pacemaker implantation, atrial fibrillation, and all-cause mortality. A 2016 study aimed to associate PR interval with AF, heart failure, and mortality in a biracial group of older adults.
In this Health ABC study, the researchers applied multivariable Cox proportional hazards models to examine the PR interval in the subjects and assess the ten-year risk of the discussed endpoints. Since a multivariable model was being used, it included clinical, demographic, and anthropometric variables in addition to heart risk factors.
2722 participants were analyzed between the ages of 74±3 years. Almost 52% of the participants were women, and 41% were black. Significant effect modification was not identified by race. Post multivariable adjustment, the increase in PR interval was associated with a 13% increased ten-year risk of heart failure.
Further, there was a 13% increased risk of incident atrial fibrillation. For a PR interval greater than 200 ms, there was a 46% higher chance of incident heart failure. But surprisingly, in this study, a prolonged PR interval wasn't associated with increased all-cause mortality.
